Share
Peripheral iridotomy laser is used in the treatment of primary angle closure disease. This disease is associated with the narrowing of the drainage angle, restricting aqueous drainage from the eye. Laser PI helps to reduce the risk of angle closure (sudden rise of intraocular pressure) and reduced risk of glaucoma (optic nerve damage).

Short term effects of laser PI include: visual blurring, photosensitivity, transient intraocular pressure rise, temporary redness, mild bleeding at the site of laser and corneal oedema. The effects can last 24-72 hours after the procedure.
Long term effects of laser PI include: cataract formation, visual dysphotopsias (glares, halos, lines, spots). These side effects are rare (< 2%). The majority of visual dysphotopsias are likely to resolve after 6 months, indicating that patients adopt or learn to ignore images. In very rare circumstance Aqueous Misdirection syndrome can complicate this procedure. Other rare complications include cystoid macula oedema (swelling of macula) and retinal haemorrhage.
What is Aqueous Misdirection Syndrome?
Aqueous Misdirection Syndrome is the phenomenon of forward movement of the iris lens diaphragm and shallowing of the anterior chamber. This causes a rise in intraocular pressure (IOP) as it closes the drainage of aqueous. This is an ocular emergency.
It is seen more commonly in small and short eyes (axial length< 21mm) and higher hypermetropic refraction (> +6DS). It can occur post surgery, post glaucoma laser, trauma or inflammation.
The underlying mechanism is unknown but thought to result from aqueous misdirected into posterior segment instead of normal flow into anterior chamber. This creates a fluid build up in the posterior chamber and results in forward movement of the iris- lens diaphragm and closure of the drainage angle resulting in high IOP.
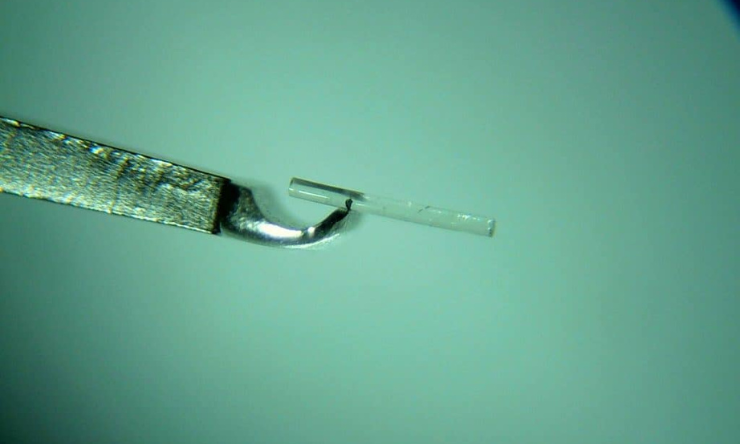
Treatment involves laser peripheral iridotomy (to exclude pupil block) and medications including cycloplegic drops to dilate the pupil and glaucoma drops to lower IOP. If this fails to treat the condition, then definitive surgical intervention involves pars plana vitrectomy.