Share
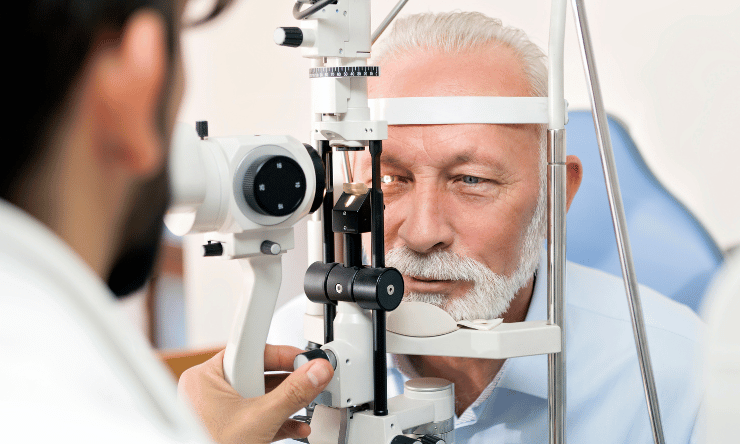
Specially-trained optometrists can deliver selective laser trabeculoplasty (SLT) safely for glaucoma, a paper published in Eye by Moorfields Eye Hospital and UCL’s Institute of Ophthalmology has revealed, taking on a significant clinical load and working autonomously to ease the burden on the eye health system.

During the past decade, glaucoma care in the UK has changed dramatically, with more non-medical ophthalmic practitioners involved. As such, optometrists and other non-medical professionals have been delivering laser treatments in the Hospital Eye Service (HES), and in 2022 SLT was elevated to a firstline option for patients following the LiGHT study findings.
A key feature of the UK’s National Health Service is that most glaucoma units actively involve non-medical ophthalmic practitioners in enhanced and advanced roles; hospital optometrists participate in nearly 90% of glaucoma clinics nationwide. One survey indicated up until 2020, optometrists regularly delivered SLT in 14 glaucoma units in the UK compared to one unit in 2016.
Meanwhile in Australia, optometrists are prohibited from offering SLT or similar laser therapies in any setting. In New Zealand, the optometry scope was recently expanded so certain practitioners can perform Nd:YAG laser for capsulotomy and/or peripheral iridotomy in an approved hospital setting, but not SLT.
However in the UK, there has been no standardised national training framework for non-medical clinicians to deliver laser therapies, with apprenticeship-style training varying between units in the country.
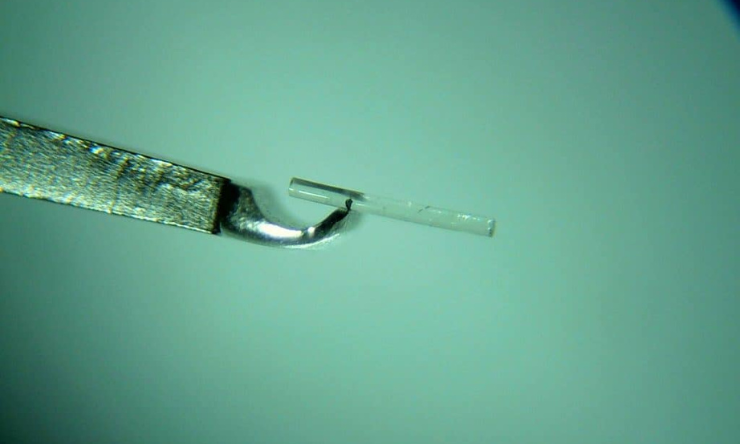
A new training program, which was the focus of this study, included six glaucoma-specialist optometrists across 240 laser procedures. Each had already been awarded the College of Optometrists Higher Certificate in Glaucoma and were independent prescribers, and were put through a three-stage course.
An audit of the results revealed:
- Performance – a total of 100% compliance with procedures was observed.
- Safety – out of 240 procedures, one eye (0.4%) developed post-laser corneal haze and one eye (0.4%) developed cystoid macular oedema; both resolved with the appropriate treatment without a permanent effect on vision. A total of 9 eyes (3.7%) had an IOP spike. There were no sight-threatening adverse events.
“The audit performed at Moorfields Eye Hospital for six glaucoma-specialist optometrists having undertaken the structured course indicates that optometrists deliver safe treatments, whilst adhering to local protocols,” the study said.
“IOP spikes, defined as an IOP > 30 mmHg, occurred in 3.7% of performed procedures. This is higher than 1% reported for the LiGHT trial, where an IOP spike was defined as a post-laser increase in IOP larger than 5 mmHg. Differences in definitions and pre-treatment IOP are likely related to the IOP spike incidence differences between the two populations. The safety of non-medical delivery of SLT has been previously described in the UK and is comparable to that reported for ophthalmologists. However, it is worth noting that the procedure has been delivered by optometrists in the US for some years.”
From the early results, the study authors said trained optometrists following the relevant clinical protocols can deliver safe laser treatments.
“Despite an initial investment of time, trained optometrists can take on a significant clinical load, working autonomously,” they said.
“Further publications on the efficacy of optometrist-delivered SLT will follow, aiming to enrich the evidence base of non-medical ophthalmic laser delivery.”
This article has been republished courtesy of Insight News.