Share
With the rising numbers of patients diagnosed with glaucoma – and oversubscription of public ophthalmology departments – the Glaucoma Community Collaborative Care Program (G3CP) at the Royal Victorian Eye and Ear Hospital (Eye and Ear) in Melbourne is designed to alleviate some of this pressure.
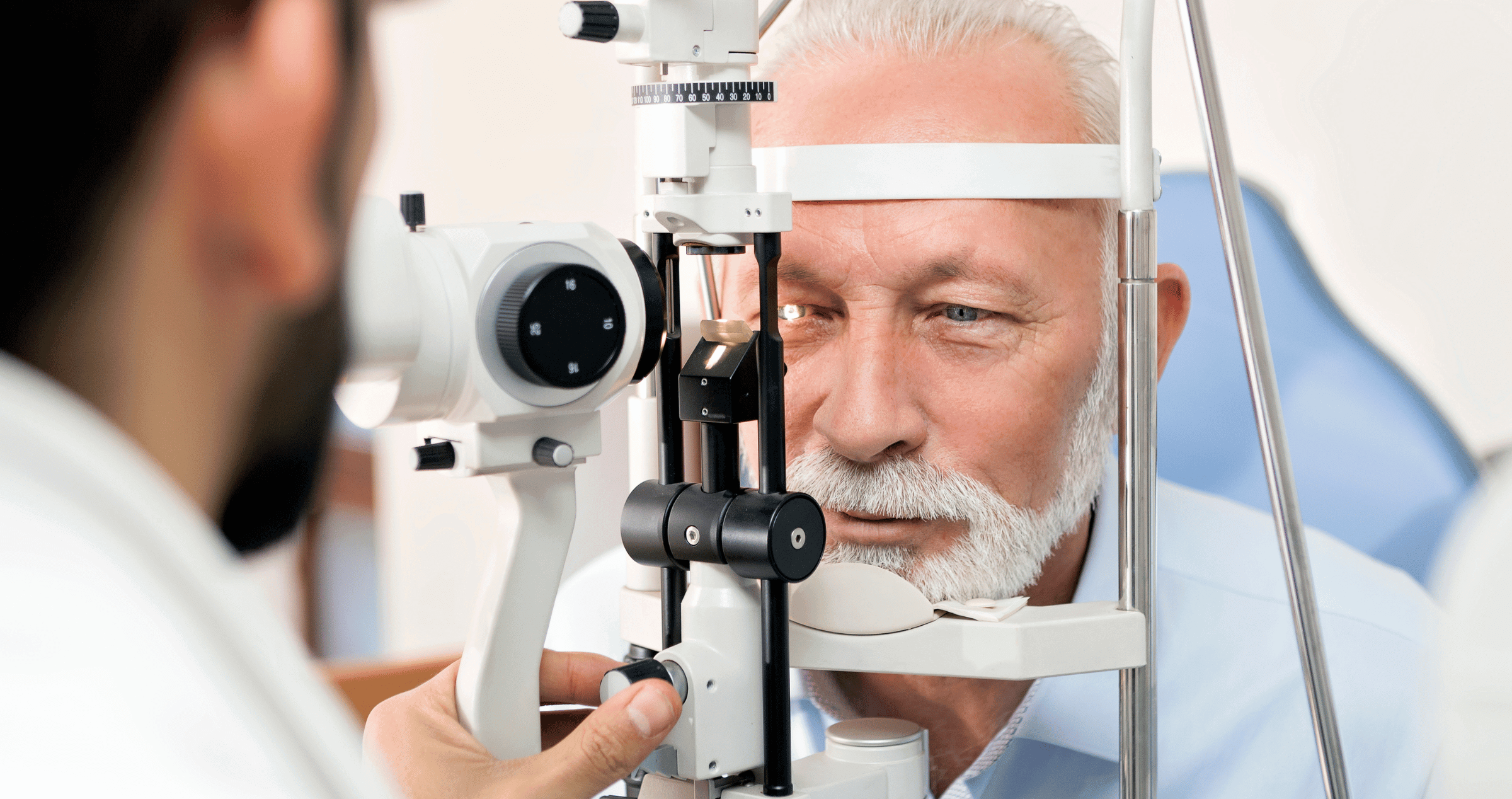
The Glaucoma Unit at the Eye and Ear provides more than 12,000 outpatient appointments a year, but there are still challenges with demand for services exceeding capacity. Established in 2018, the G3CP aims to ease this demand at the same time as ensuring patients receive appropriate and timely care. It is the largest program of its kind in Australia and has proven successful with a high degree of patient and practitioner satisfaction.
The program focuses on low-risk or suspect patients with stable glaucoma who need to remain under the care of an ophthalmologist and require close monitoring, but do not need to come to hospital clinic for every appointment.
The hospital has partnered with community optometrists who are recruited to provide care in geographical areas with high demand. Instead of having to attend the hospital for glaucoma monitoring, the clinical assessment is performed by the participating optometrists with the results of testing forwarded to the hospital and reviewed by a glaucoma specialist.
After the initial pilot program, which demonstrated safety, effectiveness and high patient and clinician satisfaction, the program is continuing to expand, with an additional 20 optometrists recently recruited.
Dr Catherine Green, AO, head of the Glaucoma Unit and ophthalmology lead of G3CP says the program has been shown to be very safe and effective. It allows patients easier access to appointments because the public system is oversubscribed by a substantial amount with low-risk patients often having their appointments delayed.
A defining characteristic of G3CP is its affordable delivery of eyecare services which allows it to make a difference in patients’ lives, particularly in a cost-of-living crisis.
“I think a key strength of our program is the informed consent, because some patients do have a small out-of-pocket expense that needs to be discussed with them while participating optometrists provide as low cost care as they can,” Green says.
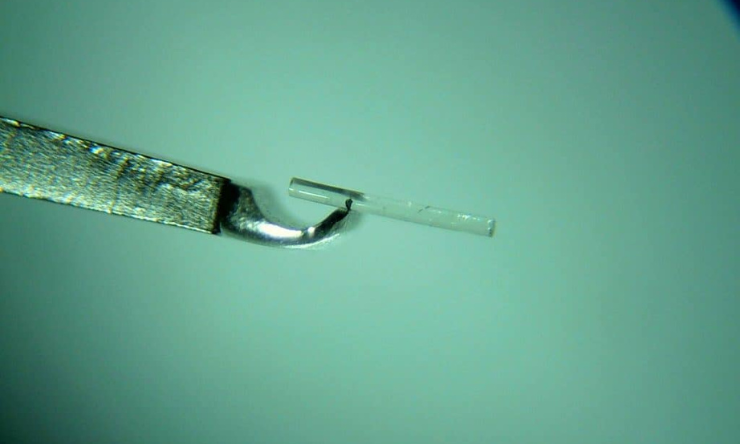
In adherence to RANZCO glaucoma collaborative care guidelines, G3CP recruits optometrists through an expression of interest. They are required, at minimum, to have a means of applanation tonometry, optic disc imaging, and access to visual field testing.
Patients are assessed in clinic by a glaucoma specialist, and those that are stable are deemed suitable for G3CP. From then on, community-based optometrists can monitor IOP and prescribe medication, working within specific guidelines. If a change in treatment is required, they will defer to the Eye and Ear for a decision.
“It means G3CP patients don’t need to see an ophthalmologist every time they get an eye check. And this is in keeping with the RANZCO Glaucoma Collaborative care guidelines,” Green says.
Through the program, patients enjoy convenience and peace-of-mind, while optometrists enjoy an expanded scope-of-practice.
“There’s a very high acceptance from patients that they actually preferred seeing a local optometrist for some of the visits knowing they are still under the supervision of the glaucoma clinic and glaucoma specialists, and very high satisfaction from the optometrists in that they enjoyed seeing slightly more complex patients,” Green says.
“A key component has been continuing professional development opportunities for the participating optometrists so they have access to the glaucoma doctors at the hospital and are also part of a community of practice all doing the same thing.”
This article has been republished courtesy of Insight News.