Share
Glaucoma is a lifelong condition, so you need to ensure you're comfortable with everyone in your support network and feel confident about the decisions made regarding your eye health. It begins with choosing the right eye care professionals for yourself and establishing trust in your specialists’ expertise.

Confident and knowledgeable patients are more likely to understand and adhere to their ongoing treatments and management plans, and therefore more likely to save their eye health and maintain their quality of life.
From my clinical experience, as well as from the conversations with patients supported by Glaucoma Australia, there is often quite a bit of uncertainty or anxiety when it comes to any upcoming appointments.
As a patient educator, my goal is to help all patients understand how important it is to not only attend their appointments, but to take an active interest in their own eye health. We want them to have confidence in their eye care professional, we want them leaving an appointment feeling well informed, and we want them feeling empowered that they have their glaucoma under control.
The entire process can sometimes be very overwhelming and you are not alone in feeling this way, so I encourage you to ask the questions, the better the knowledge you have about your eye health, the more confident you will feel about your treatment plan.
Whether it be your first or a follow-up, we want you to feel as prepared as you can be. There are many questions you can ask during your appointments depending on your circumstances.
It does help to write out any questions ahead of time, and your optometrist or your ophthalmologist will gladly address to your questions, you just have to ask. On the Glaucoma Australia website we have a checklist that you can download here.
Asking questions
If you are preparing for your first appointment, it helps to know the answers to the following questions;C
Do I actually have glaucoma? - getting tested for glaucoma does not always result in a simple yes or no answer - you may have narrow angles, you could have ocular hypertension, or you could remain an ongoing glaucoma suspect.
If the answer is yes you should ask;
- what type of glaucoma do I have?
- do I have optic nerve damage?
- what treatments are available to me?
- what are my short-term and long-term management plans for follow-up visits or an existing diagnosis?
If you are preparing for a follow-up appointment, it helps to know the answers to the following questions;
- is my glaucoma stable?
- how is my eye pressure this visit?
- is there any progression on my test so you've got your OCT test and your visual field test?
- are there any changes to my current treatment do I carry on with my current eye drops?
- are there any changes to my long term management plan?
- are you thinking of laser or surgery down the track for me?
Most glaucoma patients are on eye drops. If you get prescribed new drops on the day, or you may have some questions about the existing ones it helps to ask questions such as;
- how long will I need to take these drops for?
- what do I do if I forget them?
- are there any side effects to be aware of?
- what do I do if I'm concerned about the side effects - do I stop them, do I contact the clinic, do I make an urgent appointment?
In the event you are told it's time for laser or surgery, as eye drops alone may not be enough to lower your eye pressure, your list of questions might will most likely be longer.
Your specialist will likely give you time to think about it, but to help with your decision you will need to know the following;
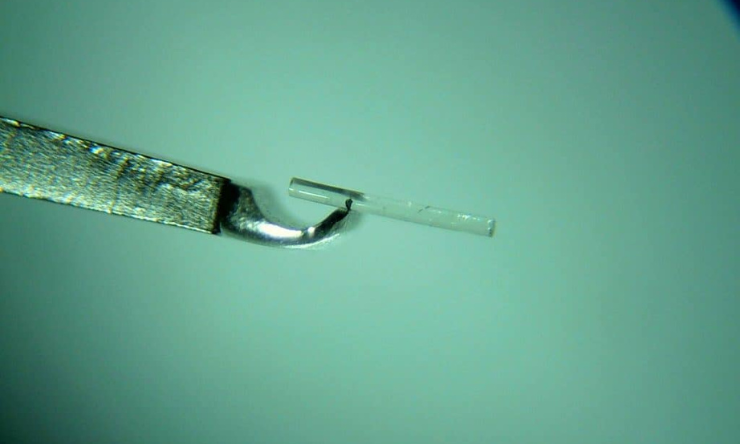
- what is the name of the procedure?
- how soon the procedure has to be done?
- how will the procedure help you and for how long - are we talking months, are we talking years?
- what risks are involved and are you at a higher risk?
- what is cost of the procedure?
- what other options do you have if you decide not to go ahead with this one ?
- will you still need your glaucoma drops afterwards?
It is important that patients have a clear understanding of all the glaucoma tests, not just the eye pressure tests, there are also visual field tests and OCT scans, so it is important to understand the following;
- why is it done
- what does it show
- why are they often repeated.
This will hopefully help you feel less nervous about the outcome of your tests, simply by having a clearer understanding of what the results mean for you, and how it impacts your treatment plan.
Many glaucoma patients have been through at least one appointment where they have felt like nothing new happens. In this case, try asking questions such as;
- why were there no changes?
- what does that mean for me?
- is it a good thing?
- is it a bad thing?
In most glaucoma cases, when it says there's no changes, it's a good thing and it probably means your glaucoma is stable and your treatment is working.
It is important to remember that glaucoma is a progressive condition. This means that any test results can change over time, and the only way to stay on top of it is by attending your appointments on a regular basis.
Other preparations
There are several other considerations when preparing for any eye specialist appointment, and I would like to share some other helpful hints on how to prepare for your appointment and what to expect when you're there.
Firstly, decide how you will be getting to your appointment and back again. In the event that you are administered eye drops to dilate your pupils, it may be wise to have someone to assist you. Alternatively, and if you know from a previous procedure, you may only need to bring along your sunglasses to lessen the light sensitivity, and if safe to do so, catch transport when you are ready.
To ensure that your appointment runs smoothly and you get the most from your visit, consider bringing the following with you;
- your referral from your GP or optometrist - this is needed for new patients and also for return patients if your previous one has expired
- your Medicare card, private health care, pension card, veteran affairs card, or any other helpful cards you might have
- credit card or cash - if you are aware of a gap you have to pay on the day
- any previous tests you have had with other eye care professionals - these may help to compare results
- a list of your most recent medications, including the dose if possible
- your medical history - if you are new to the clinic it will help to have a report as well as family history of any known health conditions
- any allergies and/or side effects - it is a good opportunity to discuss these as there may be potential for tailoring your treatment around these
- don’t forget to take any glasses you may use for reading etc.
- also, it is a good idea to bring reading or audio material in the event you encounter longer waiting times.
During your appointment
Aim to arrive at least 10 minutes before your appointment time, just in case any extra paperwork needs to be completed. Please be patient and allow a minimum of two hours for your visit. Your appointment time indicates the approximate time your testing will begin.
Tests may be performed by an officer or an ophthalmic nurse. Once the testing is completed all your results should be prepared for review by the time your ophthalmologist is ready to see you.
Your appointment may be over well ahead of the two hour allocated time, as staff are always working very hard behind the scenes to get all patients out as soon as possible.
However, various factors will determine the timings of your appointment;
- there may be an emergency case ahead of you
- perhaps there are more patients than usual waiting for tests on the same machine you're to be tested on, or
- perhaps your eyes might take longer to dilate.
It is important that adequate time is allocated to all patients as needed, depending on the individual results for the day more testing may be needed. A specialist would not request extra testing if it wasn't needed, so please be prepared in case an extra test is needed, or for more accurate results you could be repeating a test already done.
Testing
Very often patients ask me for tips on how to survive the visual field testing. The main thing to understand is how important it is. It's a long test, and it’s not fun for the patient or the person setting it up, but it's vital for monitoring your visual field to ensure we are on the right track for your treatment and the progression.
Even for patients that have had this test numerous times, they may still feel apprehensive and wonder how they can prepare better, or do better in the test if they try harder. An important thing to remember about this is to be as comfortable as you possibly can.
The better the patient is at doing the test the quicker it actually is. Communicate with the person setting it up for you, if you are uncomfortable during the test let the orthoptist or the nurse know, they're there to actually make you feel as comfortable as possible and you're actually going to get better results by doing so.
A few considerations to assist in making the visual field test quicker and more accurate are;
- firstly, you should determine if you require the chair to be adjusted – the chin rest is quite high making it hard to blink and breath
- blink, breathe, and just look straight ahead at the lights – it is so important to blink normally, if you don’t your eyes may get watery and this will affect your vision
- if you are prone to getting dry eyes during a test, you may request some lubricating eye drops
- if you need to communicate during the test you can hold down the buzzer – any time you need to ask something, or to cough, sneeze, etc.
- just focus on just getting it right while still relaxing.
You might have been made aware that you are having your eyes dilated, but sometimes they can spring this on you. It greatly depends on the individual, if you're a first-time patient and you don't know what it feels like to have your pupils dilated, it is wise to have transport organised.
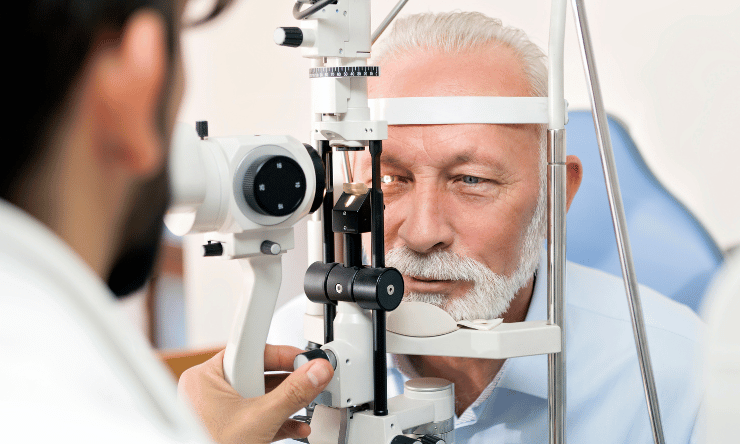
Dilation allows the ophthalmologist to have a good look at your macular, your retina, and your optic nerve on the microscope, so it is another very important process for monitoring your progression.
You should always wait after dilation before you get back into a vehicle. You may wait around for an hour or so, as it does eventually go down. With dilating drops there are stronger ones, and weaker ones - you can let them know if you are planning on driving, and especially if you were not prepared, they can administer the weaker drops.
Double drops in some eye examinations or a laser treatment are sometimes needed. In this case two to four hours is generally needed but it does depend, for example, brown eyes get affected differently to blue eyes. Don’t take the risk if you are uncomfortable, just wait around to see how you go.
After your appointment
Hopefully all went well and you have left the clinic feeling reassured and well informed. In case you forget to ask a question or if you need clarification on something you are always welcome to contact Glaucoma Australia we endeavour to answer your questions, or advise you of any next steps. We are also more than happy to go over the outcomes of your last appointment to help you better understand your diagnosis and your treatment.
The diagnosis of any health condition can be overwhelming and glaucoma is no different. By attending all your eye health appointments and with the correct treatment plan as prescribed by your eye care professional, you can save your vision from glaucoma to maintain your quality of life. Glaucoma Australia is also here to provide you with ongoing education and support throughout your journey with glaucoma.
There are a few ways to get support;
- our free support line
- web chat on our website
- message via Facebook messenger or Instagram, or
- one of the Facebook support groups we have