Share
Since his retirement from clinical work, Prof Peter Watson has been Honorary Consultant Eye Surgeon at Addenbrooke's University Hospital Cambridge and Moorfields Eye Hospital London. With Dr John Cairns, he pioneered trabeculectomy surgery, still the most common form of surgery for glaucoma.
The decades-old procedure remains the gold standard of treatment for many glaucoma patients. It was the first glaucoma surgery shown to be consistently effective and at a time when eye drops were ineffective and had terrible side effects, it revolutionised glaucoma treatment. Fortunately things have improved considerably since then and fewer people need surgery.
From my time firstly as a glaucoma Fellow and then as consultant ophthalmologist in Cambridge, I got to know Peter as a colleague and friend. I had the privilege of treating some of his original patients who had undergone trabeculectomy surgery. Some had their surgery over 40 years ago and still have good vision and intraocular pressure control. As Chair of the Cambridge Eye Trust, he was not only an invaluable source of wisdom when it came to glaucoma but a tireless fundraiser to maintain research activities at Cambridge. This is a role in which he continues to be outstandingly successful. On behalf of Glaucoma Australia, I was very pleased to ask him for his personal reflections on development of the surgery and its current role in the treatment of glaucoma.
As one may expect, there are many opinions on when glaucoma surgery is necessary and when is the appropriate time in relation to other treatments. Glaucoma Australia recommends you discuss all treatment options with your ophthalmologist so you can work together to have the best and safest treatment possible.
Cambridge in 1965 had no active surgeons. Dr John Cairns and I were appointed to the city at the same time to be confronted with a huge number of untreated glaucoma patients. The only medications available to this stable, white, stoical population at the time were diamox or pilocarpine and eserine made up in the local pharmacy without preservatives. Those who took these diligently were seriously handicapped by the side effects.
We decided the only solution to the problem was surgery; but what surgery? We had both worked for Mr Henry Stallard who had developed a highly complicated operation, which combined all the surgical procedures performed at the time, and it worked. It was, however a difficult and slow procedure.
With much thought and consumption of beer in the local pub after work we decided that the guarded filtration was the key. John felt that only the trabecular meshwork needed to be removed. I felt that it would be easier surgically, and perhaps more effective to include the scleral spur. We decided to perform 100 of each technique and compare the results. They were near enough identical (Table 1.)1.
| Results of the first 216 trabeculectomies comparing the anterior and posterior approaches.Complete 12 month follow up 1967 -1968. | |||
| Anterior JEC | Posterior PGW | ||
| Total patients | 115 | 101 | |
| Average fall of IOP | 12.3mmHg | 9.0mmHg | p<0.01 |
| Pressure remaining >24mmHg post operation | 7 (6%) | 11(11%) | NS |
| Shallow AC | 19 (16.5%) | 18(18%) | NS |
| Hyphaema | 16 (15%) | 28(28%) | p<0.05 |
| Progression of cataract | 26 (23%) | 6 (6%) | p<0.001 |
Table 1.
Twenty years of follow up confirmed its effectiveness in adult open angle glaucoma on the white population2.
Why then, with such good results is trabeculectomy not used everywhere and for everyone, assuming competent surgical technique especially as it has been shown that better control (pressure and visual field) is obtained both in those with low visual field loss and in those patients with advanced visual field loss at presentation. (P=0.0006)3? The problem is to persuade patients with no symptoms that any treatment for glaucoma, especially surgery which carries risk is warranted.
Unfortunately using medication, especially those containing preservatives such as benzylconium chloride damages the conjunctiva4 and significantly reduces the success rate of subsequent surgery (Fig1.); hence the necessity for the introduction of other agents into the surgery which in turn increases the complication rate and the hunt for alternative procedures.
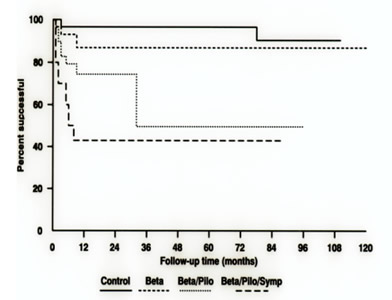
Fig 1: Success rate of trabeculectomy preceded by different medication regimes
Old habits die hard it seems5 but every patient is different. My personal conclusion after years of experience is that the best option is that anyone with an IOP greater than 28 mm Hg and field loss at presentation should be offered trabeculectomy without any prior medication of any sort. If the pressures are lower than this, non-preserved drops can be tried before any intervention such as laser trabeculoplasty. Multiple drug regimens reduce the chances of successful surgical intervention, including trabeculectomy
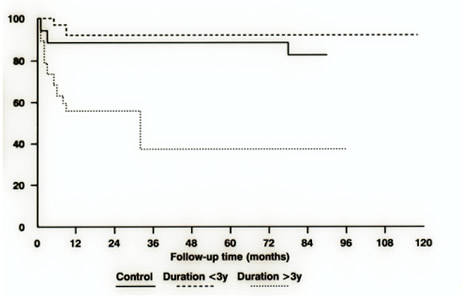
Fig 2: Surgical success rates over time