Share
This article reviews the different IOL options for use in glaucomatous eyes, the factors that need to be considered when selecting the right lens, and what outcomes patients might expect.

Cataract surgery provides an excellent opportunity to enhance the quality of life for patients with glaucoma. Advances in intraocular lens (IOL) technology can now provide greater spectacle independence in selected patients and maximise quality of vision. However, to achieve optimal outcomes, careful consideration and counselling are necessary to match the right IOL technology to a patient’s condition and expectations.
It is estimated that approximately one in five people undergoing cataract surgery have glaucoma or ocular hypertension. Both cataracts and glaucoma are conditions that increase with age.1 Treatment with glaucoma eye drops2 and filtration surgery3 may also accelerate cataract development.
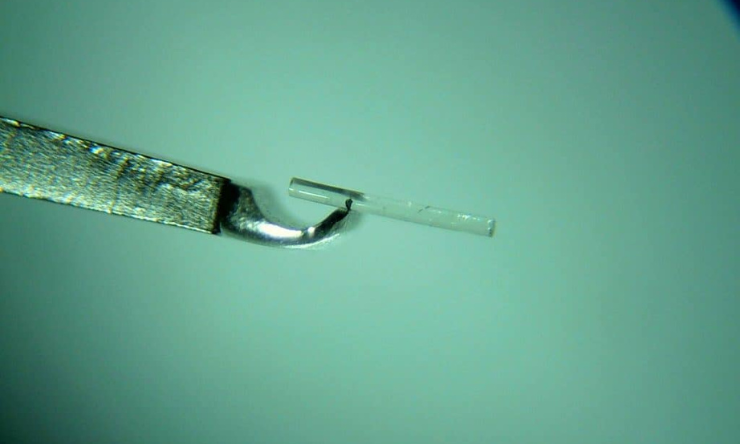
It is important to remember that for people with glaucoma and cataract, both conditions need to be adequately addressed. The introduction of cataract surgery combined with minimally invasive glaucoma surgery (MIGS) now allows both conditions to be treated in a single procedure. However, historically, the pathophysiological changes in glaucoma have limited IOL choices for people living with the condition. Fortunately, new presbyopia-correcting IOL technologies are providing greater options for people with glaucoma who wish to reduce their dependence on glasses.
Changes in glaucoma that influence IOL selection
Glaucoma is associated with a loss of contrast sensitivity and this loss correlates with the degree of structural and functional glaucomatous damage.4 Contrast sensitivity may even be affected in early glaucoma and is preferentially lost to a greater extent than visual acuity.5 Decreased contrast sensitivity can cause visual symptoms and is a common cause of visual complaints, even where visual acuity is normal. In addition, contrast sensitivity decreases with age.6 This is important when considering IOL selection. Because certain types of IOLs split light, less light reaches the retina and contrast sensitivity is reduced.
As glaucoma patients have impaired contrast sensitivity, special consideration must be given to the impact of the IOL on contrast sensitivity as there is a risk of compromising the quality of vision, especially in low-light conditions.
In addition to contrast sensitivity, there are other changes that can influence IOL performance. Eyes with glaucoma tend to have smaller pupils than non-glaucomatous eyes7 and this can impair the performance of pupil-dependent IOL technologies. As well as poor pupil dilation, conditions such as pseudoexfoliative glaucoma may be associated with zonular weakness. This can lead to IOL decentration that can impair the performance of presbyopia-correcting IOLs and induce higher order aberrations.
The performance of presbyopia-correcting IOLs is affected by the quality of the tear film and ocular surface. Dry eye and ocular surface disease are more common in patients with glaucoma, especially in those taking multiple medications containing preservatives. Careful attention should be paid to the ocular surface and co-existing dry eye and lid conditions, such as blepharitis, treated pre-operatively. This is critical not only for IOL performance post-operatively but also to obtain the most accurate biometry measurements that will be used for surgical planning and IOL power selection pre-operatively. For patients with intolerance to glaucoma eye drops or where drops are ineffective, I discuss combining cataract surgery with a MIGS procedure to reduce medication burden and to help promote a healthy ocular surface that may in turn lead to better quality vision.
Lastly, glaucoma is a lifelong and potentially progressive condition. Before surgery, I evaluate many clinical factors including the stage of glaucoma, IOP control, adherence with therapy, optic disc appearance, retinal nerve fibre and ganglion cell analyses, visual field loss, risk factors for progression, and co-existing retinal/macular disease, to determine IOL suitability not only now, but in the future.
Progression after IOL implantation could result in unwanted visual symptoms and compromise quality of vision. For this reason, I avoid multifocal or extended depth of focus (EDOF) IOLs in patients with advanced disease or central visual field defects, as well as those at high risk of progression. Patients must be carefully counselled on the outcomes they can expect and what lens is best suited to their individual circumstances.
IOL options and how to choose the right lens
The choice of IOL is one of the most important decisions in cataract surgery as it will influence the quality and range of vision a patient may expect after the procedure. To select the correct lens, we need to understand the benefits, risks, and safety profile of each lens in relation to pre-existing glaucomatous change (and concurrent eye conditions), visual expectations, patient motivation, and occupational/recreational visual needs.
Monofocal IOLs
A monofocal IOL is an option for all stages of glaucoma. Providing excellent distance vision when aimed for emmetropia, these lenses require spectacle correction for intermediate and near activities. With greater use of tablets, digital automobile dashboards, and smartphones in everyday life, patients can find this frustrating. Monovision is a way to reduce but not eliminate spectacle dependence,8however it is associated with a loss of depth perception and suboptimal vision at intermediate distances.9 For this reason, suitable patients motivated to reduce their dependence on glasses may be better served with monofocal plus, EDOF, or multifocal IOL technology.
I use monofocal IOLs for patients who are happy to wear spectacles for intermediate or near activities, or if there is (or there is a significant future risk of) advanced or central visual loss where the use of an EDOF or multifocal IOL may further reduce contrast sensitivity and compromise the quality of vision, especially for low-light tasks. For patients with pseudoexfoliation and weak zonules, a standard monofocal may be preferable as IOL power is the same from the centre to the edge and it will induce less aberrations if there is decentration in the future.
Toric IOLs
Patients with glaucoma may have astigmatism, especially if they have undergone trabeculectomy.10Toric IOLs can safely and predictably reduce astigmatism and provide better uncorrected vision in patients with glaucoma.11 Correcting even low levels of cylinder can improve the quality of vision. Toric lenses are available for all types of IOL and can be used in all stages of glaucoma. These lenses can be combined with astigmatically-neutral MIGS procedures but should be used with caution in combined cataract surgery with trabeculectomy because of the unpredictable degree of surgically-induced astigmatism with conventional filtration surgery.12 Similarly, caution should be applied when considering toric IOLs in patients with small pupils and zonular weakness due to the risks of misalignment, decentration, and dislocation.
Extended Depth of Focus IOLs
Extended Depth of Focus IOLs are an entirely new category of presbyopia-correcting lenses designed to improve range of vision, especially intermediate vision, with few photic phenomena and less loss of contrast sensitivity compared to traditional multifocal IOLs. As such, EDOF IOLs may be an option for people with glaucoma who wish to reduce their dependence on glasses, but otherwise may not be candidates for a multifocal IOL. Unlike multifocal IOLs, which create distinct focal points, EDOF lenses provide a continuous range of high-quality vision from distance into intermediate and even near, although not providing as much near vision as a multifocal. However, targeting the nondominant eye for -0.5D can enhance binocular near vision for patients who demand superior near vision while retaining good binocular distance vision. EDOF IOLs provide excellent intermediate vision, which is ideal in today’s digital lifestyle with increasing use of computers, tablets, and smartphones. These lenses have a low incidence of dysphotopsia and few night vision symptoms.
I offer EDOF technology to patients who have early to moderate, stable glaucoma with only peripheral field defects and absolutely no loss of sensitivity in the central 10 degrees. Patients with secondary glaucoma or co-existing retinal pathology are poor candidates and may be better managed with a monofocal IOL.
Multifocal IOLs
Multifocal IOLs provide distance, intermediate, and near vision with a high level of independence from glasses. However, as mentioned, these lenses split light and reduce contrast sensitivity which could theoretically impair the quality of vision in eyes with glaucoma, especially in low light level settings. While new generation multifocal IOLs have improved light transmission and less impact on contrast sensitivity then older generations, these lenses should be used with caution and on an individual basis for people with glaucoma. There is limited data on the use of multifocal IOLs in glaucomatous eyes and existing studies are small.13 As such, I tend to restrict the use of these lenses to patients with primary angle closure, ocular hypertension, and stable pre-perimetric or early glaucoma.
Conclusion
For people with glaucoma and cataract, these are exciting times. The introduction of MIGS has enabled us to simultaneously address both cataract and glaucoma in a single procedure. For many people, this allows them to reduce their medication burden or even stop taking glaucoma eye drops. Now, with refractive cataract surgery and new IOL technology, we can also reduce dependence on glasses by correcting presbyopia and/or astigmatism at the time of lens extraction. Ultimately, these interventions help us maximise a patient’s quality of vision and improve their quality of life.
This article has been republished courtesy of www.mivision.com.au
References
1. Leibowitz HM, Krueger DE, Maunder LR, et al. The Framingham Eye Study monograph: An ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973-1975. Surv Ophthalmol 1980;24:335–610.
2. Leske MC, Wu S-Y, Nemesure B, et al. Risk factors for incident nuclear opacities. Ophthalmology 2002; 109:1303–1308.
3. Feiner L, Piltz-Seymour JR, Study CIGT. Collaborative Initial Glaucoma Treatment Study: a summary of results to date. Curr Opin Ophthalmol 2003;14:106–111.
4. Hawkins AS, Szlyk JP, Ardickas Z, et al. Comparison of Contrast Sensitivity, Visual Acuity, and Humphrey Visual Field Testing in Patients with Glaucoma. J Glaucoma 2003;12:134–138.
5. A A, I B-W, M W, et al. Abnormalities of central contrast sensitivity in glaucoma. Am J Ophthalmol 1979;88:205–211. Available at: https://doi. org/10.1016/0002-9394(79)90467-7.
6. McKendrick AM, Sampson GP, Walland MJ, Badcock DR. Contrast Sensitivity Changes Due to Glaucoma and Normal Aging: Low-Spatial-Frequency Losses in Both Magnocellular and Parvocellular Pathways. Investigative Opthalmology Vis Sci 2007;48:2115.
7. Park JW, Kang BH, Kwon JW, Cho KJ. Analysis of various factors affecting pupil size in patients with glaucoma. Bmc Ophthalmol 2017;17:168.
8. Greenstein S, II RP. The Quest for Spectacle Independence: A Comparison of Multifocal Intraocular Lens Implants and Pseudophakic Monovision for Patients with Presbyopia. Semin Ophthalmol 2016;32:1–5.
9. Wilkins MR, Allan BD, Rubin GS, et al. Randomized Trial of Multifocal Intraocular Lenses versus Monovision after Bilateral Cataract Surgery. Ophthalmology 2013;120:2449- 2455.e1.
10. Delbeke H, Stalmans I, Vandewalle E, Zeyen T. The Effect of Trabeculectomy on Astigmatism. J Glaucoma 2016;25:e308–e312.
11. Brown RH, Zhong L, Bozeman CW, Lynch MG. Toric Intraocular Lens Outcomes in Patients With Glaucoma. J Refract Surg 2015;31:366–372.
12. Ong C, Nongpiur M, Peter L, Perera SA. Combined Approach to Phacoemulsification and Trabeculectomy Results in Less Ideal Refractive Outcomes Compared With the Sequential Approach. J Glaucoma 2016;25:e873–e878.
13. Kumar BV, Phillips RP, Prasad S. Multifocal intraocular lenses in the setting of glaucoma. Curr Opin Ophthalmol 2007;18:62–66.