Share
With an ageing population and more than 300,000 people estimated to be living with glaucoma in Australia – half of those completely unaware they even have the condition – new surgical interventions, translational research projects and innovative care models are emerging to soften its impact.
One such development is the transition from traditional therapeutic avenues as first line treatment to medication free alternatives. As issues with compliance and a reduction of life-quality are commonly associated with eye drops, the industry is exploring new avenues that are revolutionising the treatment landscape.
A current snapshot of glaucoma management shows that newly diagnosed glaucoma patients are increasingly being treated with selective laser trabeculoplasty (SLT) as a first line treatment. This is based on evidence from the LiGHT trial; a landmark study demonstrating that starting with SLT as first line therapy compared to medical therapy exhibited greater intraocular pressure (IOP) control and thus patients were more likely to be medication free.
Currently, nearly three-quarters of these patients are still medication free, six years after SLT. More importantly, people treated with laser first have a lower rate of losing peripheral vision and a much lower rate of needing to go on to have further invasive surgery.
One surgeon who has been following the data closely is Dr Nathan Kerr, of Eye Surgery Associates in Melbourne, a researcher at the Centre for Eye Research Australia (CERA) and one of Australia’s most well-credentialled glaucoma specialists.
“In recent years, SLT has emerged as the preferred first line approach for open-angle glaucoma and ocular hypertension, offering a more patient-centric solution. This method significantly reduces the challenges associated with adherence – a notable obstacle, as numerous patients find daily eye drop application challenging. Moreover, SLT avoids the potential side effects commonly associated with eye drops and reduces the risk of field progression and need for incisional glaucoma surgery. By integrating SLT as our initial treatment strategy, we effectively address these concerns, enhancing overall patient care and outcomes,” Kerr says.
He says that the industry is witnessing a profound paradigm shift in the approach to treating glaucoma.
“A decade ago, the standard protocol involved initiating treatment with medical therapy. Typically, if a single agent proved insufficient, we escalated the treatment, often incorporating up to three different medications before even considering laser therapy. However, now we have a deeper understanding of the benefits of SLT.”
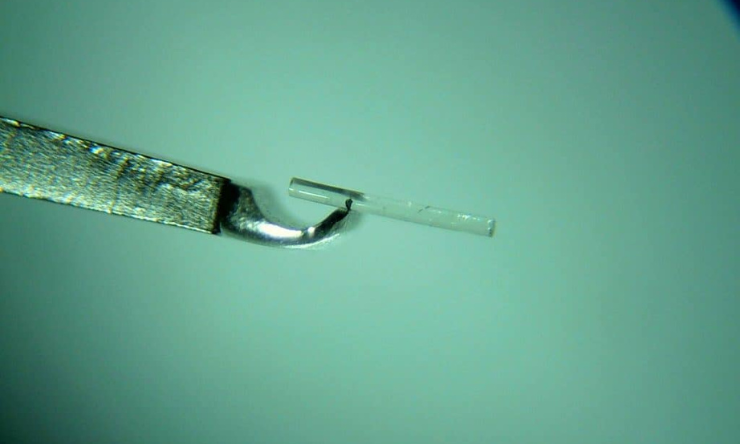
Kerr completed the first surgery in Australia using the iStar MINIject minimally invasive glaucoma surgery (MIGS) device late last year since it became commercially available. He says the device represents a significant advancement in MIGS, which is a surgical option for patients where medical therapy is ineffective or poorly tolerated.
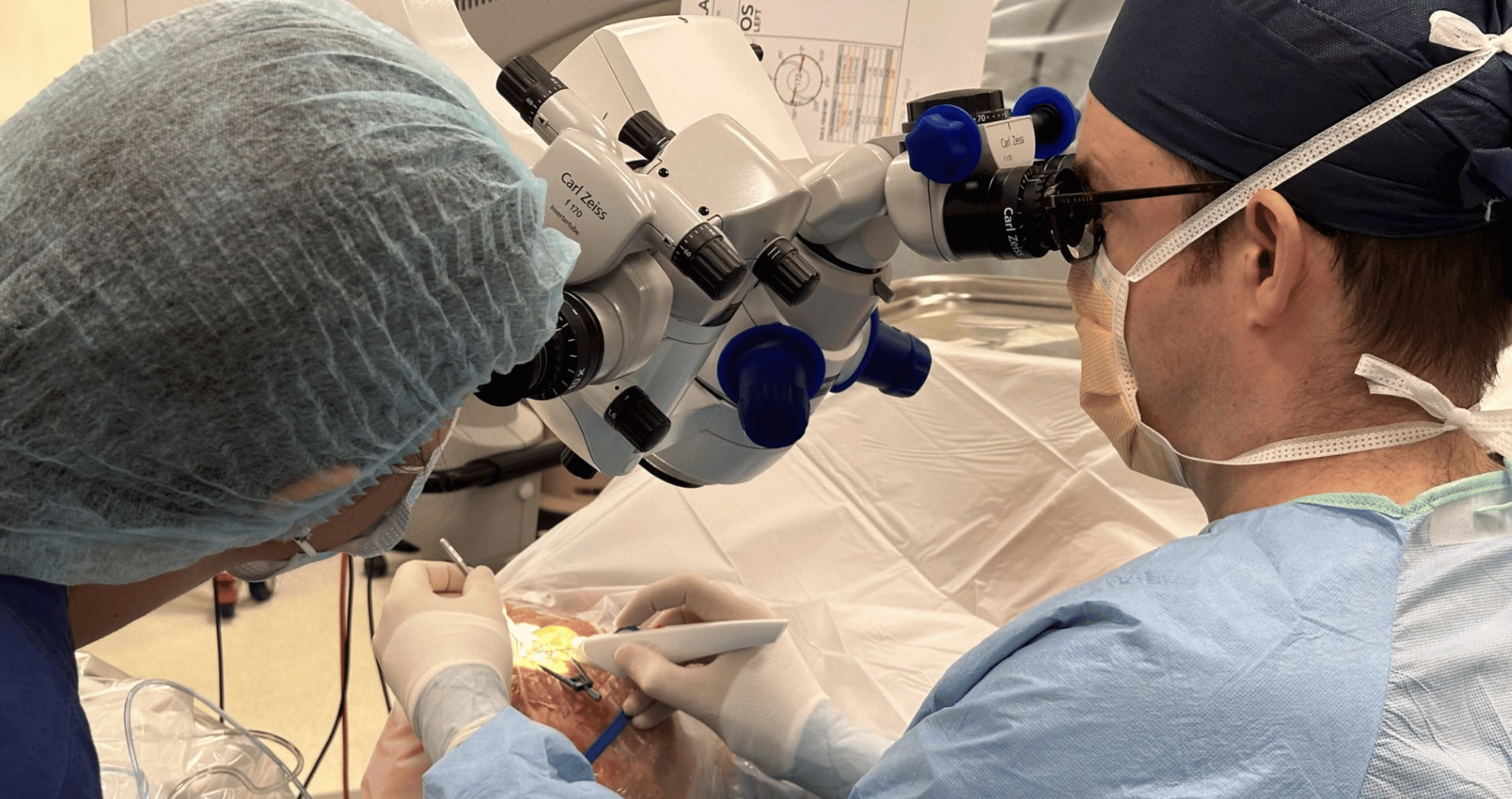
“MIGS is playing a pivotal role in reducing the need for trabeculectomy. While trabeculectomy is a highly effective procedure, it’s also considerably invasive and demands an extended recovery period. The current market offers a range of MIGS devices, supported by a robust and continually growing body of evidence underscoring their safety and efficacy. This advancement has revolutionised the management of glaucoma,” Kerr says.
Ultimately, the goal of these procedures is to extend beyond preventing vision loss; with the aim to enhance overall quality of life. This involves minimising reliance on medications, lowering the risk of side effects, and ensuring a swift recovery so that patients can return to their normal activities.
“These innovative technologies are not just about treating a condition; they’re about offering a superior patient experience and significantly improving their quality of life. It’s an incredibly exciting time in the field of ophthalmology,” Kerr says.
There are two natural drainage routes inside the eye: The conventional pathway (Schlemm’s canal) – which the iStent, Hydrus, and iTrack utilise – has been shown to be safe and effective; and the uveoscleral pathway which is the focus of the MINIject. This procedure creates a pathway for aqueous to flow into the suprachoroidal space, which effectively lowers IOP. Additionally, the suprachoroidal space is less prone to scarring compared to traditional filtration surgeries, possibly leading to more sustained IOP control.
“Unlike MIGS devices which primarily facilitate aqueous outflow through Schlemm’s canal and into the episcleral venous system, the MINIject offers an alternate approach. It bypasses the episcleral venous pressure floor, which inherently limits the extent to which IOP can be reduced. This bypass mechanism allows the MINIject to potentially achieve lower IOP levels, granting it a unique advantage in certain clinical scenarios,” Kerr says.
When performed with routine cataract surgery, Kerr says that Schlemm’s canal and MINIject procedures boast good safety profiles that are very similar to that of standalone cataract surgery.
MIGS preserves the ocular surface by avoiding glaucoma drops so the patient’s ocular surface remains intact which is important for intraocular lens (IOL) performance. Therefore, the outcomes of cataract surgery are improved.
“The integration of MIGS during routine cataract surgery not only maintains an excellent safety profile but also enhances the overall surgical outcomes. By reducing or eliminating the need for glaucoma drops, MIGS plays a crucial role in improving the ocular surface which is vital for optimal IOL performance. Patients benefit from a dual therapeutic approach that addresses both cataract and glaucoma in a single, streamlined procedure,” Kerr says.
“As we approach a decade of utilising MIGS in Australia, our understanding and expertise in this field have grown significantly. Globally, the body of data on MIGS devices has surpassed the 10-year mark. Notably, the HORIZON study on the Hydrus Microstent stands out as not only the largest trial specifically focused on MIGS but also one of the most extensive in the field of surgical ophthalmology,” Kerr says.
“Initially, there was a degree of uncertainty surrounding the safety and efficacy of MIGS. However, with nearly 10 years of clinical experience and robust data, we’ve effectively addressed these concerns. The current focus is now on ensuring that this advanced care is accessible to all patients who could benefit from it.”
Kerr says the trajectory of the glaucoma landscape not only offers a wide range of treatment options that can be tailored to patients’ needs, but provides quality-of-life that traditional methods have not been able to achieve.
“The advancements in glaucoma treatment over the past few years have been truly remarkable. While our primary objective continues to be the preservation of vision, the scope of our care has broadened significantly,” he says.
In the past, postoperative periods following conventional surgical methods often meant a prolonged recovery for patients, characterised by frequent follow-up visits, blurred vision, and eye discomfort. Kerr welcomes the shift towards newer techniques that facilitate a quicker and more comfortable recovery process.
“Being able to provide these advanced treatment options and witnessing the positive impact on our patients’ lives is exceptionally rewarding. It’s an indication of meaningful progress in our field, enhancing both the effectiveness of our treatments and the quality of life for our patients,” he says.
This article has been republished courtesy of Insight News.