Share
Glaucoma is a disease where the pressure inside the eye is often high. Over time, it leads to the death of ganglion cells. Ganglion cells are the nerve cells sending electrical signals to the rest of the brain for further analysis of visual scenes.

The optic nerve - made up of nerve fibres of the ganglion cells will also die over time. Thus, glaucoma results in blindness in which the peripheral part of the visual field is affected first, eventually results in tunnel vision. Among other risk factors, high intra-ocular pressure (IOP) can be lowered and managed by drugs. Lowering IOP tends to slow down disease progression. One candidate tested scientifically was cannabis.
The use of cannabis has been around for thousands of years. There are over 500 different chemical compounds, 104 of these are cannabinoids, and its primary psycho-active ingredient is delta-9-tetrahydrocannabinol or THC (ElSohly et al., 2016). Cannabis has been known to temporarily lower IOP. It can be smoked where there is an increased risk of lung diseases. Hepler and Frank in 1971 reported smoking marihuana caused an average of 25% reduction in IOP of 11 subjects. Merritt and others (1980) also shown marihuana inhalation decreased IOP and blood pressure in 18 subjects with heterogeneous glaucomas. Cannabis can be orally administrated. Flach (2002) demonstrated an initial decrease in IOP after oral administration of THC capsules in all nine patients with end-stage open-angle glaucoma. Another study by Tomida and colleagues (2006) treated six patients with ocular hypertension or early primary open angle glaucoma, and demonstrated a low dose of sublingual THC temporarily reduced
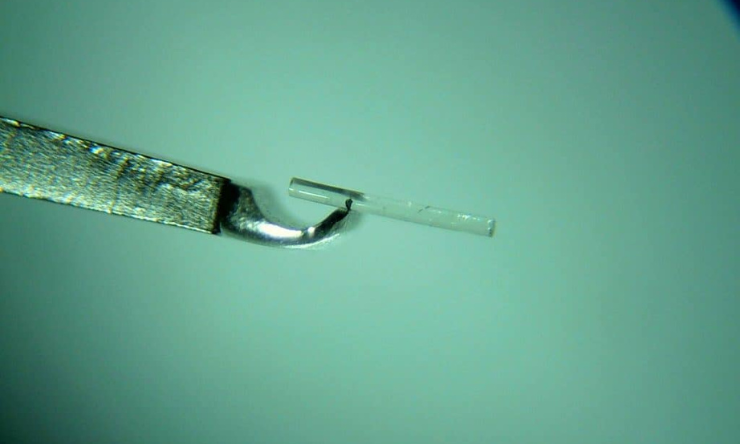
IOP. In this study, the drug was well tolerated by most patients. THC can also be applied topically to the eye, however, this method appears to be the most ineffective where irritation and corneal damage can occur (Green and Roth, 1982; Jay and Green, 1983). So how does cannabis lower IOP? It was thought that cannabis decreased aqueous humour production via cannabinoid receptor activation as shown in normal and glaucomatous monkeys (Chien et al., 2003).
The short-term benefit of lowered IOP lasting hours means patients need to consume cannabis many times a day in order to achieve a constant decrease in IOP (Tomida et al., 2006). Continuous use of cannabis could lead to addiction. Plus patients need to tolerate its side effects such as dry mouth, sleepiness, dizziness, distortion of perception, anxiety, depression, confusion, euphoria, dysphoria, disruption of short-term memory and lowering of arterial blood pressure (Flach, 2002; Tomida et al., 2006). It is important to note that all patients in the Flach’s 2002 study elected to discontinue treatment within 1 to 9 months. In most cases, therapeutic benefit did not outweigh toxicity. Another challenge of using cannabis is the development of tolerance (diminished response to a drug after repetitive usage) were observed in many subjects (Falch, 2002).
Recently, Whiting and co-workers (2015) conducted a systematic review and meta-analysis of a total of 79 trials consists of 6462 participants on medical cannabis. The National Academies of Sciences, Engineering and Medicine (2017) reviewed over 10,700 quality scientific work published since 1999 on cannabis. Both papers identified limited studies and lack of long term studies of cannabis treatments on glaucoma. Thus the National Academies concluded: “There is limited evidence that cannabinoids are an effective treatment for improving intraocular pressure associated with glaucoma”.