Share
Glaucoma is the leading cause of irreversible blindness worldwide. Intraocular pressure (IOP) control is the most important factor in preventing glaucoma progression. In patients with mild to moderate glaucoma, minimally invasive glaucoma surgery (MIGS) has emerged as a promising new treatment option.

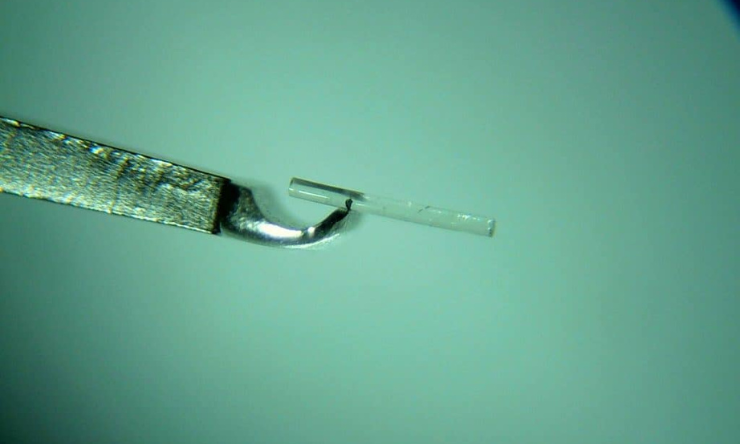
The iStent is a small medical device inserted into the eye to increase the amount of fluid drainage to lower eye pressures. Research has been conducted to determine if cataract surgery, in combination with glaucoma surgery, could be more successful in lowering eye pressures in people with Primary Angle Closure Glaucoma (PACG) than having cataracts surgery alone.
Drainage angles are narrow in primary angle closure glaucoma which results in less fluid being able to leave the eye resulting in higher eye pressures. By removing the cataract which widens the drainage angles, and by placing a drainage device in the eye to allow more fluid to leave the eye, a greater reduction in eye pressure can be achieved.
The study concluded, iStent implantation in combination with cataract surgery resulted in significantly higher rates of complete success compared with cataracts surgery alone - with a higher proportion of angle closure eyes not requiring glaucoma medications after the surgery.
In view of the potentially sight‐threatening complications, most surgeons are reluctant to perform combined surgeries in patients with medically controlled glaucoma. However, the study showed that combined Phaco‐iStent (cataracts surgery and iStent) has a favourable safety profile, and the incidence of complications was comparable with cataracts surgery alone; and no sight‐threatening complications were reported.
Reference
Chen D. Z et al. 2020, Phacoemulsification vs phacoemulsification with micro‐bypass stent implantation in primary angle closure and primary angle closure glaucoma: A randomized single‐masked clinical study, Clinical and Experimental Ophthalmology, Volume 48, Issue 4, pp. 450-461, RANZCO
< https://doi-org.ezproxy.lib.swin.edu.au/10.1111/ceo.13721>