Share
During the past decade and a half OCT has evolved from a research tool into something that is widely and routinely used by ophthalmologists and optometrists. The capability of OCT to diagnose and monitor ocular conditions has improved considerably. Machines have also become more user-friendly and affordable.
It can be used to diagnose, monitor and screen various conditions including glaucoma and macular disorders. It is slowly expanding its role in imaging the anterior segment as well as the evaluation of blood flowing in retinal vessels through the advent of OCT-angiography.
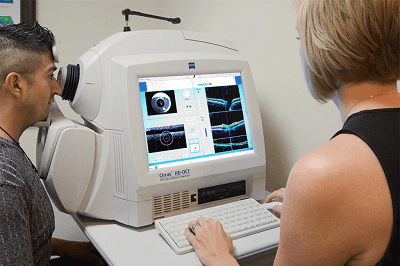 OCT allows more accurate screening, earlier diagnosis and prompt therapy resulting in greatly improved outcomes in the management of many eye conditions. It is a disruptive technology that has changed the way we practice and has replaced many routine tests.
OCT allows more accurate screening, earlier diagnosis and prompt therapy resulting in greatly improved outcomes in the management of many eye conditions. It is a disruptive technology that has changed the way we practice and has replaced many routine tests.
Certainly, there are few other tests that are currently as reliable and useful as the OCT. In addition, it is non-invasive and does not have the potential to harm the patient. It does not add a significant cost to the health care system. We have no problem with using OCT in routine clinical practice by all eye care professionals, and in fact, would encourage it.
RANZCO does not have a position on whether one group of eyecare professionals should or should not use a particular technology. This includes OCT. Ultimately it is the patient who is the focus, and therefore whatever is best for the patient should be adopted – especially if it can identify a problem earlier and manage it better.
It has been suggested that there has been overuse of it as a diagnostic tool, especially by optometrists, but we neither believe there are any indicators to suggest this is the case, nor are there any studies that have demonstrated this. There may be some false positives resulting in over-diagnosis from its use, however, these can be easily identified with no harm to a patient. Until such time as a study conclusively shows that over-diagnosis is an issue, we would rather deal with over-diagnosis than risk missing pathology. After all, it is better to be safe than sorry.
We are not sure that the recent increase in OCT use has increased the overall cost to the healthcare system, as again, we are not sure it has been studied or, if it has, we are not privy to the figures.
OCT use is not yet adopted for routine screening for diabetic retinopathy (DR) because it is yet to be validated as a screening tool for the condition, but I am sure by the time the next update of the RANZCO Diabetic Screening Guidelines is due, OCT will have an important role in the detection of diabetic macular edema. Its capability to assist in the detection of retinal nerve fibre changes, hence picking up pre-perimetric glaucoma, will go a long way in reducing visual disability and blindness.
I think there is overwhelming consensus that the regular use of OCT in clinical practice by all eye health professionals should be regarded as a positive step in the management and diagnosis of ocular disease. Used appropriately, it will undoubtedly improve outcomes for the screening, detection and management of eye conditions.
In fact, it has now reached the stage where I wonder how we managed without it.
RANZCO Guidelines
RANZCO guidelines for screening using OCT as a tool are evidence-based. One needs to differentiate between using OCT as a tool for management of the disease versus screening for it.
Whenever the evidence is strong enough, the use of OCT (or any other imaging modality or diagnostic tool) will be recommended for screening and is incorporated in the RANZCO screening guidelines for the disease.
RANZCO has developed different sets of guidelines for the three most common sight threatening diseases; age-related macular degeneration(AMD), glaucoma and DR. For these conditions, screening is extremely important since good programs – supported by evidence-based guidelines – will result in early detection, prompt therapy and better visual outcomes for the patient.
In today’s context, this is even more relevant as we have some very effective treatments for these diseases. They all work better if treatment is given early rather than late.
Referral pathways are an integral part of screening guidelines and are part and parcel of any screening program. When screening guidelines are reviewed every few years, they should reflect the current science at that time and should be modified or updated as needed.
None of the RANZCO guidelines rely entirely on the use of OCT. It is only the referral pathway for AMD management that refers to the use of OCT as being important, but only in very certain circumstances.
The pathway for glaucoma does not refer to the use of OCT, while the pathway for DR does refer to OCT use, but specifically says “OCT assessment of the macula aids the detection of diabetic macular oedema. However, its use in diabetic retinopathy screening programmes is not yet validated and therefore OCT imaging is not mandatory or recommended as part of a screening examination”.
Evidence based on research shapes the way we practise, and all these must be kept updated to maintain their relevance. Medicine and healthcare are changing quickly, and we need to keep pace with the science.
RANZCO is acutely aware of this and has committees and expert groups to ensure we rain current. This does involve a lot of work, expense and consultation, which we have been happy to contribute as an organisation to support a collaborative model of eyecare that is the best for our patients.
To put things in perspective, during the last DR guidelines review and update, RANZCO sought feedback from all stakeholders and, although there was a push for OCT to be included as mandatory in DR screening, there is still no strong evidence to state that it is necessary, so the position rains as stated above. AMD guidelines are still under review.
Overall the development of the referral pathways and guidelines has been positively received. Anecdotal feedback from RANZCO Fellows and optometrists has been very positive. Both groups are working very well together and ultimately it’s patients who see the positive impact and benefit of these measures.
In Australia, DR screening is carried out by optometrists, GPs, nurses and ophthalmologists. Any screening guidelines that are used by different groups out of necessity must have a common denominator, which outlines the basic acceptable evidence-based minimum standards that applies to all groups. OCT can certainly be used as demanded by the clinical situation. The lack of OCT on site does not mean screening cannot be carried out.
The role of OCT as a screening tool will be studied in more detail in the coming years – as will other modalities – and when the available evidence is convincing enough, the guidelines will be updated. We have seen this change over the years, such as when the gold standard in DR screening, fundoscopy was replaced by digital fundus photography.




