First line treatment for glaucoma is usually in the form of eye drops or laser therapy. When these two options are no longer sufficient or are not suitable, glaucoma surgery may be required.
Conventional glaucoma filtration surgery is effective but can be associated with significant risk factors. In recent years, a new class of treatment called ‘minimally invasive glaucoma surgery’ or ‘MIGS’ is changing the glaucoma treatment model. These procedures use tiny incisions to place microscopic devices inside the eye to lower the pressure inside the eye, aiming to reduce or eliminate the need for glaucoma eye drops or invasive surgery. More importantly, MIGS devices do not typically disturb the conjunctiva (the membranous covering of the eyeball), therefore it does not alter the success rate of subsequent glaucoma filtration surgery, if required. MIGS procedures are most commonly performed at the time of cataract surgery but some can be performed alone if required.
These procedures represent a major advance for people with glaucoma. However, they will not cure your glaucoma, reverse any damage already caused by glaucoma, or bring back any vision which has already been lost.
Types of MIGS
There are a number of MIGS procedures and they work in different ways. In the healthy eye, the amount of fluid produced is equal to the amount of fluid that drains out. However, in glaucoma the natural drainage channel inside the eye (where fluid normally drains out of the eye) becomes clogged or blocked. This results in a rise in pressure which can damage the optic nerve. MIGS procedures work by bypassing this blockage and help the fluid inside the eye drain out via different routes.
There are a number of MIGS procedures available in Australia and you should speak with your ophthalmologist to see if one is suitable for you:
- iStent inject W
- iStent Infinite
- Hydrus
- XEN Gel Stent
- iTrack Ab-Interno Canaloplasty
- PRESERFLO® MicroShunt
- Paul Glaucoma Implant
- MINIject
iStent inject W
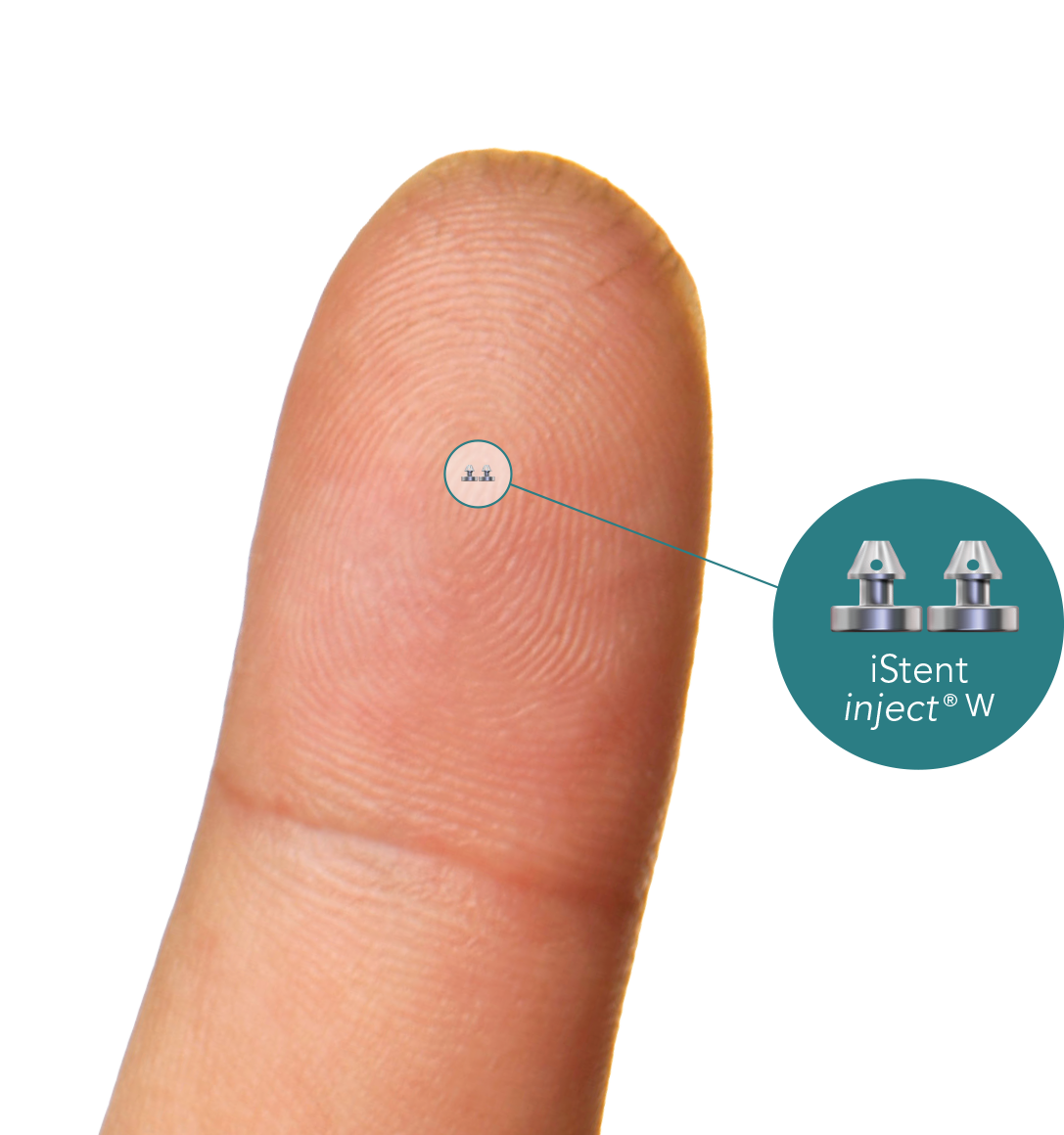
What is it?
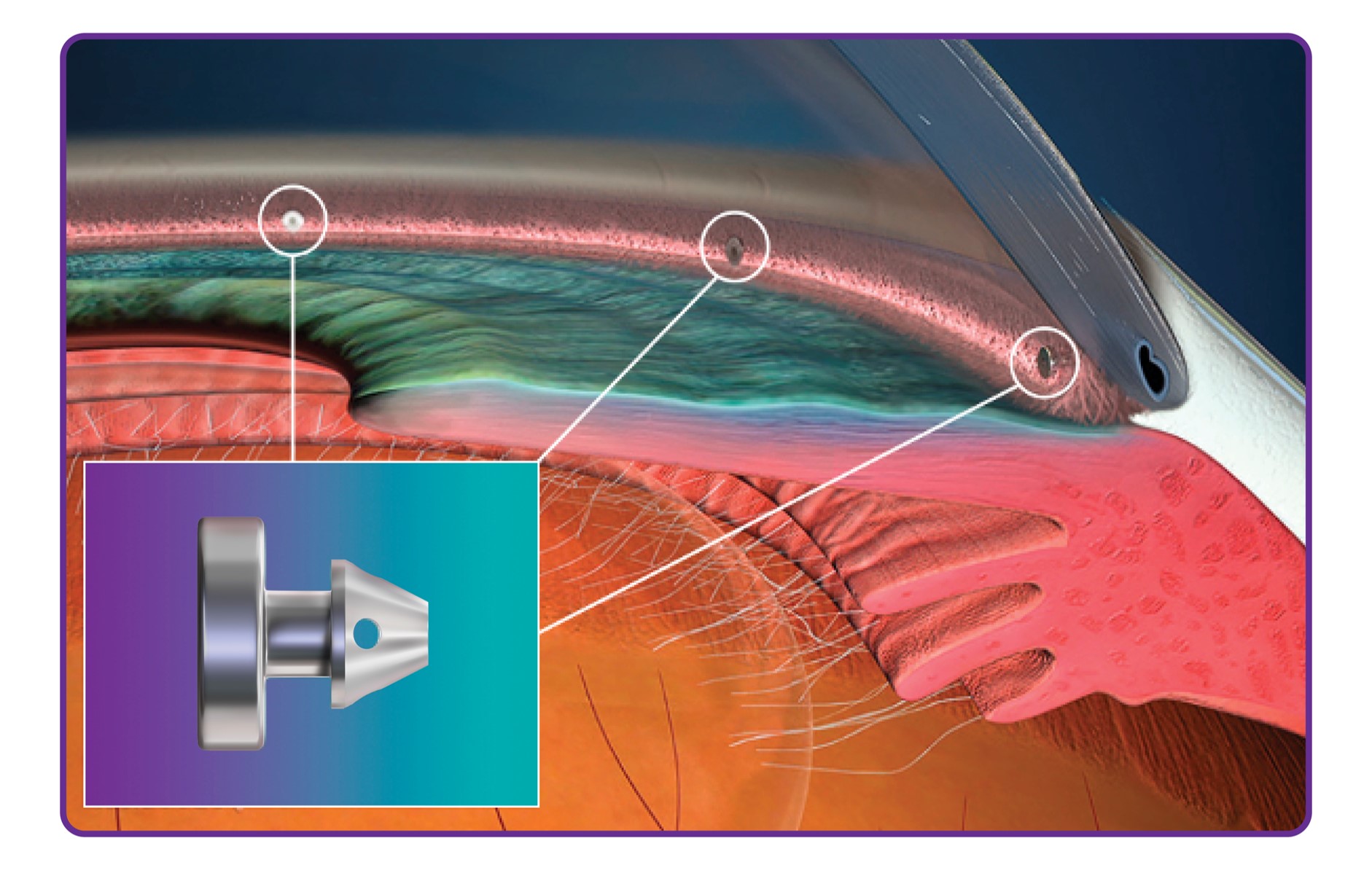
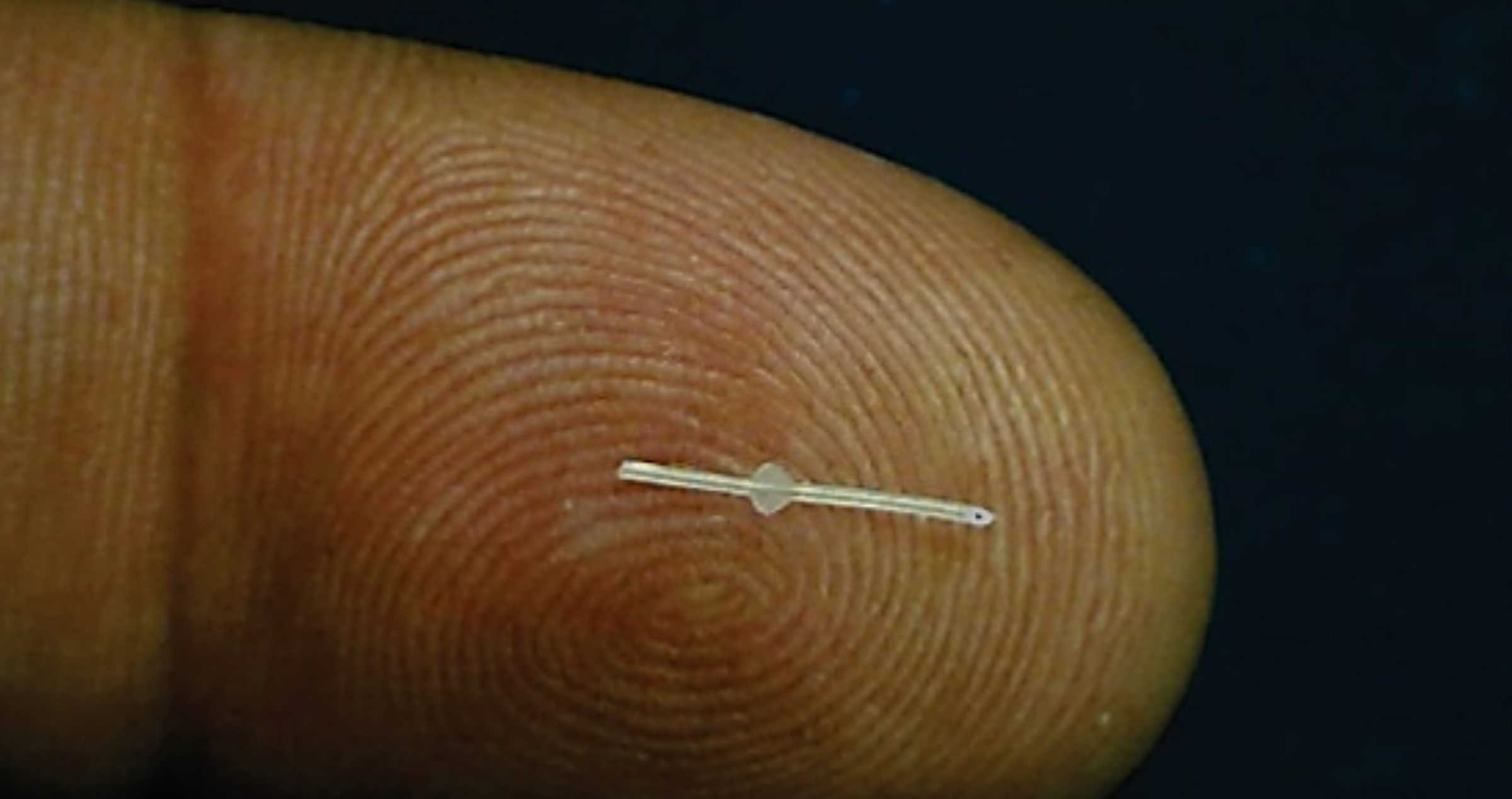
The iStent inject W is a tiny tube less than 1 mm in length made of surgical-grade titanium. The iStent inject W is inserted into the natural drainage channel inside the eye, bypassing the blockage, allowing fluid to more easily drain out. Two stents are typically inserted at the same time as cataract surgery to lower eye pressure and reduce the need for glaucoma medications.
How does it work?
These tiny stents work by bypassing the trabecular meshwork, which is presumed to be blocked in open-angle glaucoma. The fluid inside the eye therefore drains via the stents into Schlemm’s canal rather than through the trabecular meshwork.
Who is it suitable for?
The procedure is most suitable for adult patients with mild-to-moderate open-angle glaucoma treated with glaucoma eye drops who require cataract surgery. iStent inject W is not suitable for the treatment of very advanced glaucoma or where the natural drainage system of the eye is damaged. iStent inject W is also not suitable for patients with closed angle glaucoma.
What are the benefits?
The potential benefit is the lowering of intraocular pressure and possibly reducing the number of glaucoma eye drops without undergoing complex glaucoma surgery. Recovery is rapid. iStent inject W cannot be seen or felt. It is safe to have an MRI scan and X-ray following this procedure.
Before the Procedure
Your doctor will provide you with specific instructions prior to the operation. You will usually be asked to continue with all your usual medications including your glaucoma eye drops even on the day of surgery. You will likely have a period of fasting immediately before the surgery but again your doctor will provide you with the specific details
During the procedure
Your eye will be anaesthetised with a local anaesthetic injection. The procedure itself is quick and usually only takes minutes to complete. iStent inject W is delivered through a very small incision (2 mm) in the front of the eye and implanted into the drainage pathway. The two stents are implanted in different areas to maximise outflow of fluid. If combined with cataract surgery, your surgeon may choose to implant the stents before or after cataract surgery.
After the procedure
The recovery from surgery is rapid and typically no longer than cataract surgery alone. Your surgeon will prescribe some antibiotics and anti-inflammatory eye drops to apply for up to one-month following the surgery. You may be able to stop some or all of your glaucoma eye drops. However, the effect of the iStent inject W can reduce over time and glaucoma eye drops may need to be resumed.
What are the risks?
The potential risks and complications associated with iStent inject W are low. There is a small risk of bleeding inside the eye at the site of the stent implantation which often resolves spontaneously. The intraocular pressure may also increase temporarily following the procedure. Because this is an intraocular procedure, there is the small risk of potential infection inside the eye.
Are there any alternatives?
The alternative treatment options are glaucoma eye drops, laser therapy, one of the other MIGS devices, or conventional glaucoma surgery. Your doctor will be able to explain each of these and whether they are suitable for you.
iStent Infinite
What is it?
The iStent infinite is the latest addition to the iStent family. It comprises of 3 microstents, each measuring less than l mm in length and is made of surgical grade titanium.
How does it work?
The infinite is inserted into the natural drainage channel inside the eye, bypassing the blockage, allowing fluid to more easily drain out. Three stents are typically inserted at the same time as cataract surgery or as a standalone procedure and aims to lower eye pressure and reduce the need for glaucoma medications.
What are the benefits?
The potential benefit is the lowering of intraocular pressure and possibly reducing the number of glaucoma eye drops without undergoing complex glaucoma surgery. Recovery is rapid. iStents are the smallest known body implant and cannot be seen or felt. It is safe to have an MRI scan and X-ray following this procedure.
Before the Procedure
Your doctor will provide you with specific instructions prior to the operation. You will usually be asked to continue with all your usual medications including your glaucoma eye drops even on the day of surgery. You will likely have a period of fasting immediately before the surgery but again your doctor will provide you with the specific details.
During the procedure
Your eye will be anaesthetised with a local anaesthetic injection. The procedure itself is quick and usually only takes minutes to complete. iStent infinite is delivered through a very small incision (2 mm) in the front of the eye and implanted into the drainage pathway. The two stents are implanted in different areas to maximise outflow of fluid. If combined with cataract surgery, your surgeon may choose to implant the stents before or after cataract surgery.
After the procedure
The recovery from surgery is rapid and typically no longer than cataract surgery alone. Your surgeon will prescribe some antibiotics and antiinflammatory eye drops to apply for up to one-month following the surgery. You may be able to stop some or all of your glaucoma eye drops. However, the effect of the iStent infinite may reduce over time and glaucoma eye drops may need to be resumed.
What are the risks?
The potential risks and complications associated with iStent infinite are low. There is a small risk of bleeding inside the eye at the site of the stent implantation which often resolves spontaneously. The intraocular pressure may also increase temporarily following the procedure. Because this is an intraocular procedure, there is the small risk of potential infection inside the eye.
Are there any alternatives?
The alternative treatment options are glaucoma eye drops, laser therapy, one of the other MIGS devices, or conventional glaucoma surgery. Your doctor will be able to explain each of these and whether they are suitable for you.
Hydrus
What is it?
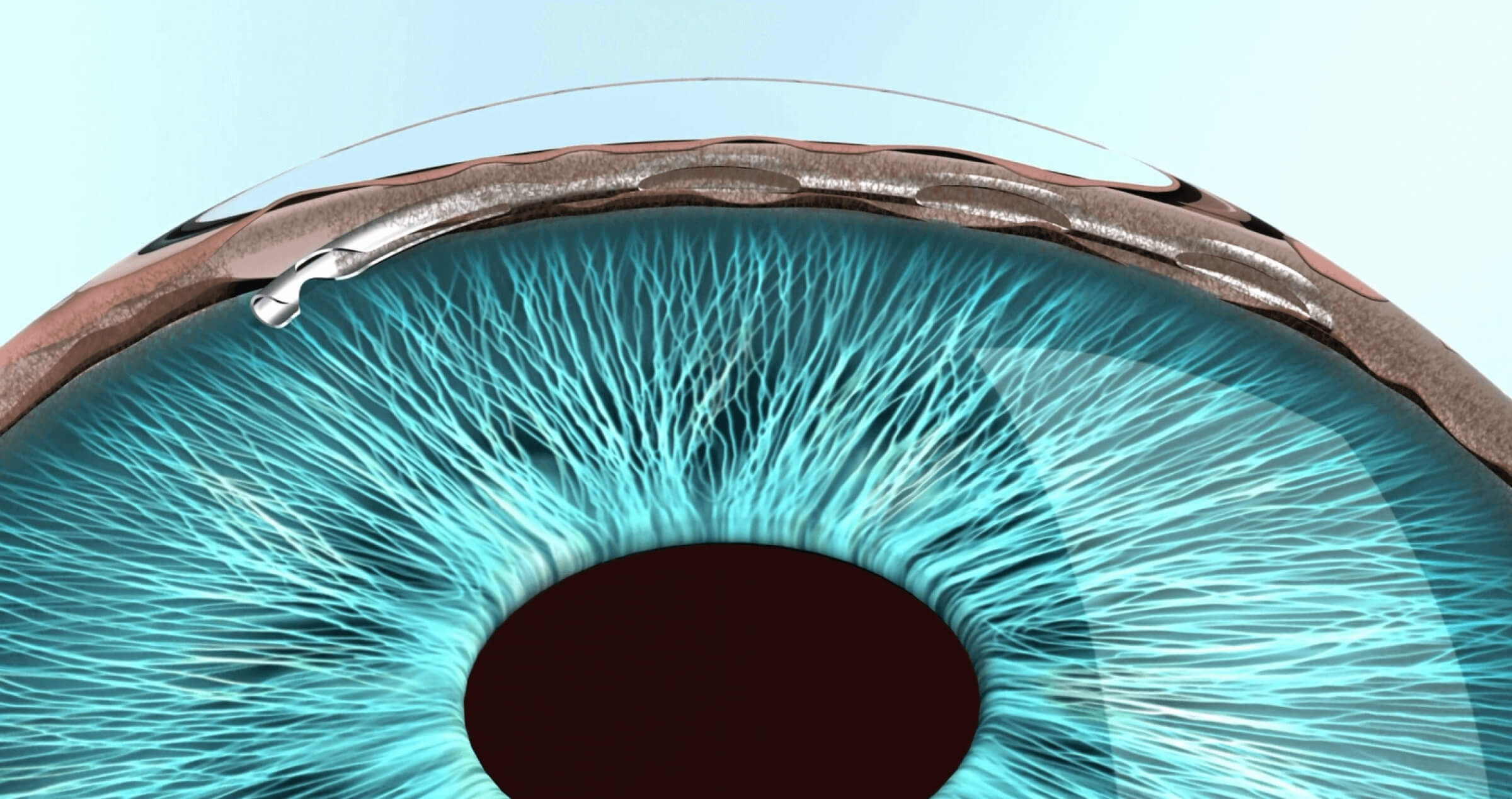
The Hydrus is a curved flexible stent approximately the size of an eyelash. It is made of a super-elastic alloy of nickel and titanium, the same material used to make stents for use in the heart.
How does it work?
Once inserted, it acts like a scaffold to widen and dilate the natural drainage channel inside the eye. It contains a small inlet to allow fluid inside the eye to enter the stent.
Who is it suitable for?
It is suitable for people with mild-to-moderate open-angle glaucoma who may require additional treatment to glaucoma eye drops and laser and/or in whom eye drops are not tolerated.
What are the benefits?
Recovery is rapid and patients may experience a modest reduction in eye pressure and/or need for glaucoma medication. The Hydrus cannot be seen or felt. It is safe to have an MRI scan in most machines following the Hydrus procedure.
Before the Procedure
Your doctor will provide you with specific instructions prior to the operation. You will usually be asked to continue with all your usual medications including your glaucoma eye drops even on the day of surgery. You will likely have a period of fasting immediately before the surgery but again your doctor will provide you with the specific details.
During the procedure
Your eye will be anaesthetised with a local anaesthetic injection. Hydrus is quick to insert and usually only takes minutes to complete. The device is delivered through a very small incision (2 mm) in the front of the eye and implanted directly into Schlemm’s canal. If combined with cataract surgery, your surgeon may choose to implant the stents before or after cataract surgery.
After the procedure
The recovery from surgery is rapid and typically no longer than cataract surgery alone. Your surgeon will prescribe some antibiotics and anti-inflammatory eye drops to apply for up to one-month following the surgery. You may be able to cease your usual glaucoma eye drops as advised by your doctor. However, the effect of the device can reduce over time and glaucoma eye drops may need to be resumed or your doctor may recommend other treatment options.
What are the risks?
The potential risks and complications associated with Hydrus are low. There is a small risk of bleeding inside the eye at the site of the stent implantation. The intraocular pressure may also increase temporarily following the procedure. There is a small risk of poor positioning or dislodgment of the stents, and this may require a return to theatre for re-positioning, removal of stents, or re-insertion of stents. Because this is an intraocular procedure, there is the small risk of potential infection inside the eye.
Are there any alternatives?
The alternative treatment options are glaucoma eye drops, laser therapy, one of the other MIGS devices, or conventional glaucoma surgery. Your doctor will be able to explain each of these and whether they are suitable for you.
Xen Gel Stent
What is it?
The XEN is a soft and flexible tube derived from porcine collagen. It is 6 mm long and nearly as thin as a strand of human hair.
How does it work?
The Xen Gel Stent works by creating a new drainage channel in the eye and drained fluid forms a small blister or bleb under the membranous covering (conjunctiva) of the eye, located on the top of the eye and covered by the upper eyelid. The bleb cannot usually be seen with the naked eye or felt. It is also MRI safe.
Who is it suitable for?
XEN implantation is typically performed by itself to lower eye pressure where medications have failed to reduce eye pressure to a safe level. However the XEN can be performed with cataract surgery for people with both advancing glaucoma and cataract, or where the drainage channel is closed. Because the XEN bypasses the natural drainage channels altogether it can be used in more types of glaucoma including where the natural drainage channel is damaged or closed.
What are the benefits?
The XEN is less invasive and offers a much faster recovery than traditional glaucoma surgery. Unlike the most commonly performed glaucoma operation, called trabeculectomy, there is no need for sutures and the return of clear vision is more rapid. The XEN has the potential to lower intraocular pressure more than iStent Inject and Hydrus and therefore can be performed on patients with moderate to advanced glaucoma. As the XEN starts to work straight away to lower eye pressure, you will be able to stop taking your glaucoma drops in the operated eye immediately after the procedure.
Before the Procedure
Your doctor will provide you with specific instructions prior to the operation. You will usually be asked to continue with all your usual medications including your glaucoma eye drops even on the day of surgery. You will likely have a period of fasting immediately before the surgery but again your doctor will provide you with the specific details.
During the procedure
Your eye will be anaesthetised with a local anaesthetic injection. A small incision will be made in the front of the eye to allow implantation of the XEN. The procedure is faster than traditional glaucoma surgery and may take approximately 30 minutes to complete.
After the procedure
Following surgery, your surgeon will prescribe some antibiotics and anti-inflammatory eye drops but you should be able to cease your usual glaucoma eye drops as advised by your doctor. You will need to attend regular follow-up appointments to monitor your eyes.
What are the risks?
XEN implantation is associated with a small risk of infection, bleeding inside the eye, and very low intraocular pressure than may lead onto choroidal effusions (collapsing of the inner layers of the eye). The stent itself has the potential to move or perforate the surface of the eye and this can result in leakage of the aqueous fluid and higher risk of infection. In this case a return to the operating theatre is required for repair.
Are there any alternatives?
Alternative treatment options include traditional glaucoma operations such as trabeculectomy and glaucoma drainage tubes. Certain types of laser therapy may also be considered.
iTrack - Ab-Interno Canaloplasty
What is it?
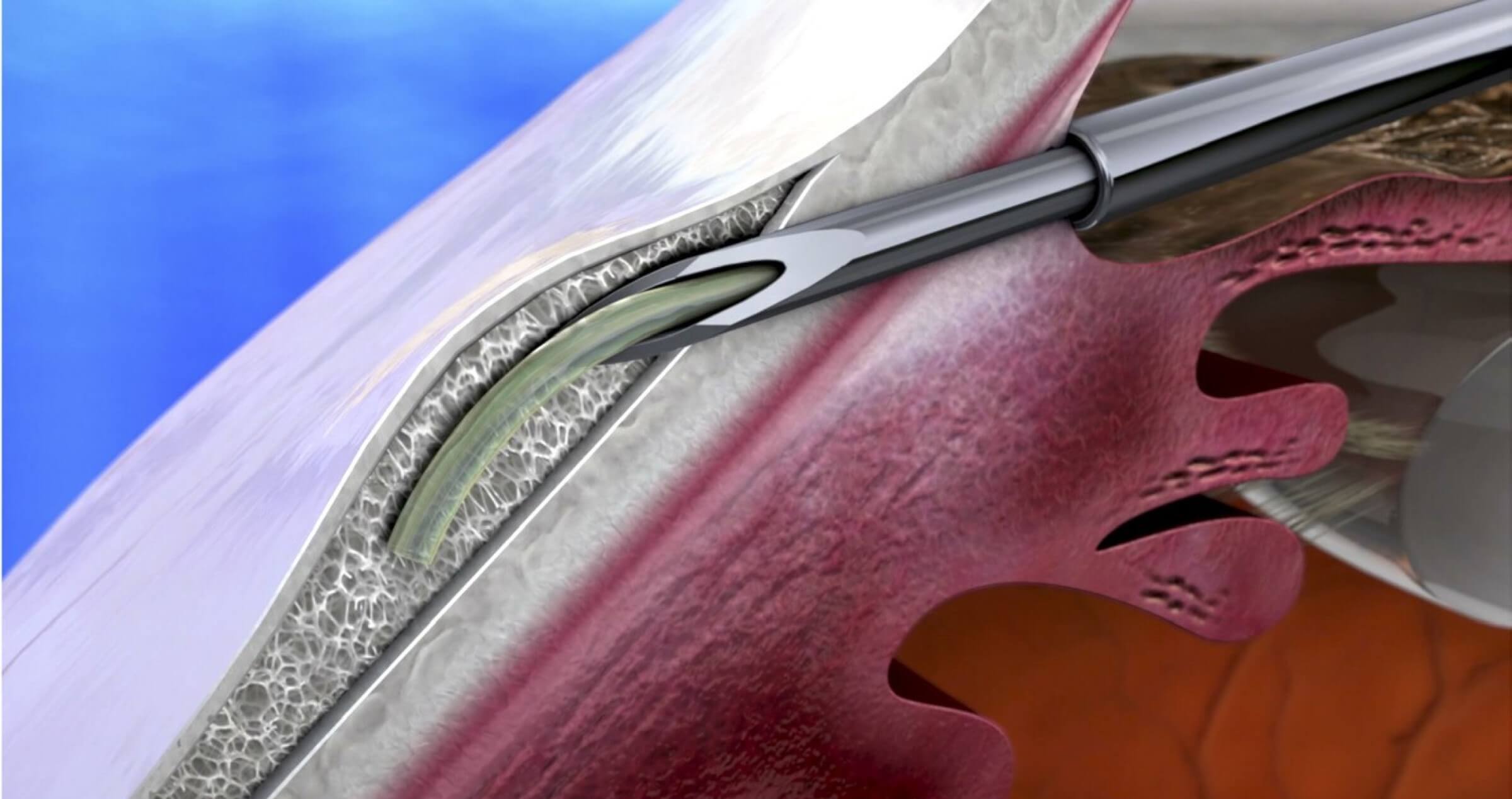
Ab-interno canaloplasty is one type of Schlemm’s canal-based surgery.
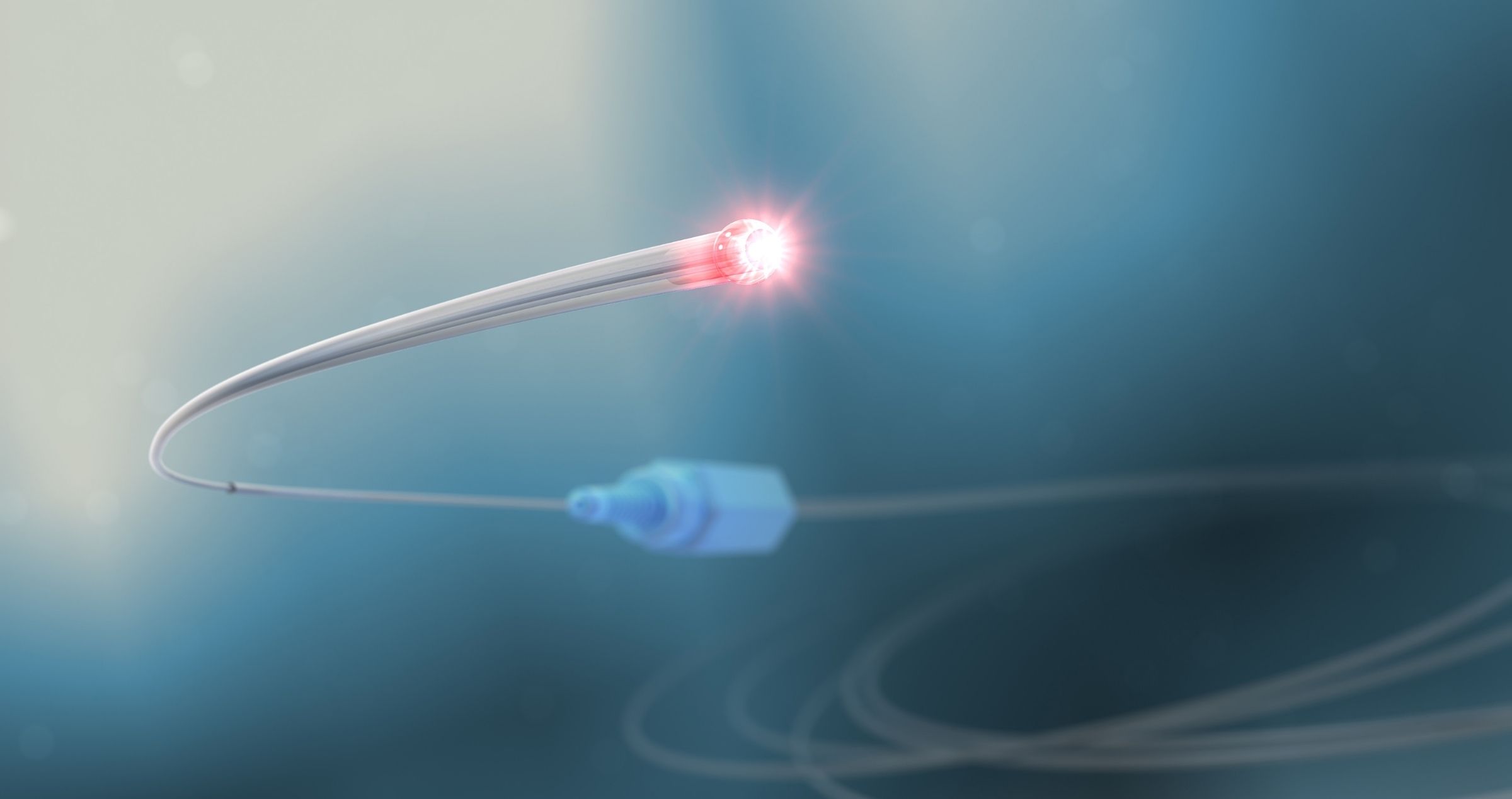
How does it work?
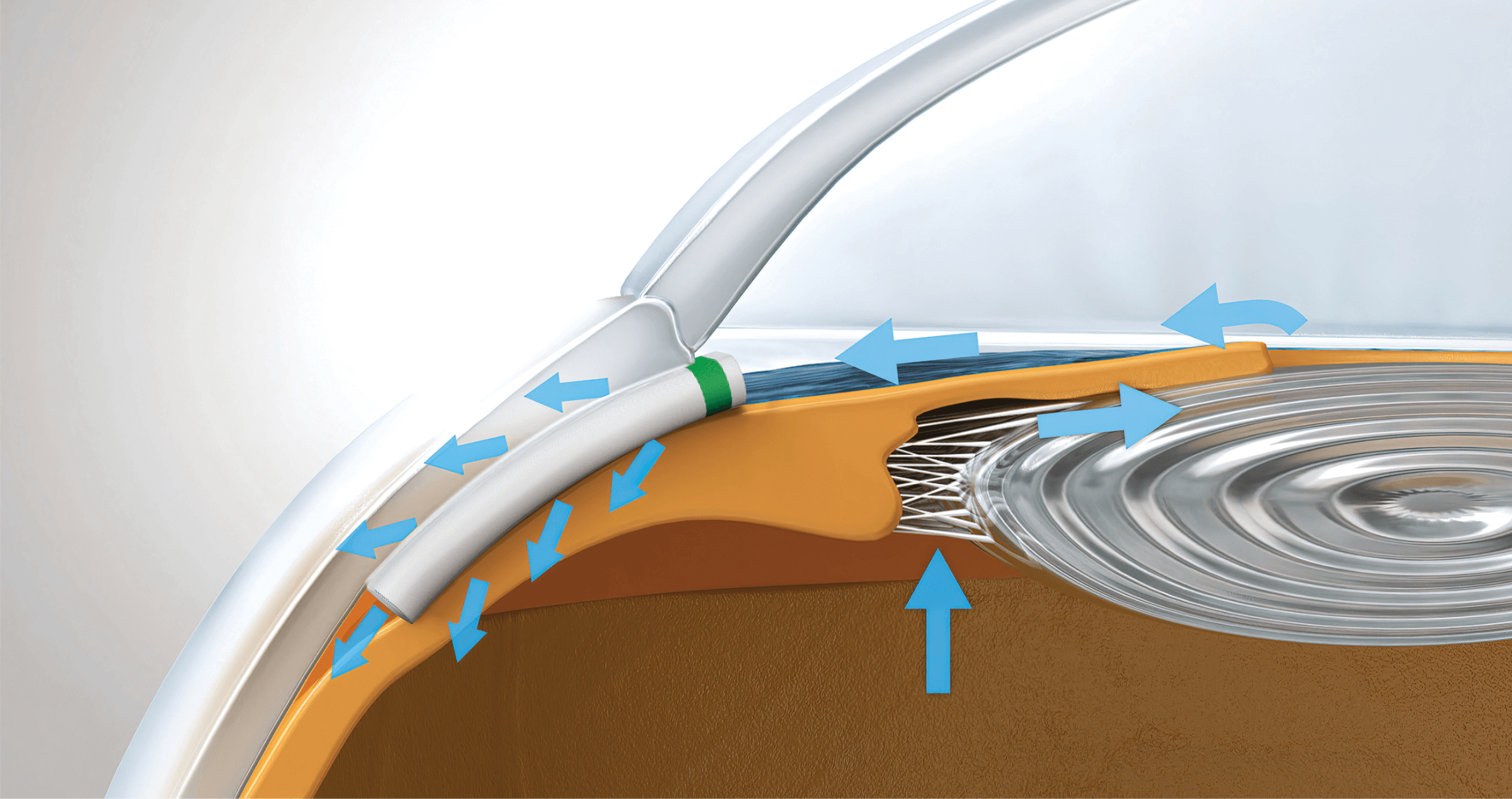
The front chamber of the eye contains roughly around 0.2 mL of clear fluid called aqueous humor, which is made by the eye every minute, of every day. Aqueous humor gives the eye “pressure”. It is also constantly flowing out of the eye out of the eye everyday, through the trabecular meshwork, a type of filtration membrane circumferentially encircling the iris. The trabecular meshwork drains most of the aqueous humor into Schlemm’s Canal. From Schlemm’s Canal aqueous humour flows into the aqueous collector channels and then onto the blood circulation.
Who is it suitable for?
Typically, in open angle glaucoma, the mechanism for increased intraocular pressure (eye pressure) is resistance to aqueous humor outflow from the trabecular meshwork. Schlemm’s canal-based surgery tries to overcome or bypass this resistance to outflow either at the trabecular meshwork or Schlemm’s canal level.
Not all patients are suitable for iTrack ab-interno canalopasty. It is preferable for patients to have an open angle glaucoma which includes pseuodoexfoliative glaucoma and pigmentary glaucoma types. This can be determined by your ophthalmologist.
What are the benefits?
Ab-interno canaloplasty aims to increase aqueous humor outflow from the eye into the aqueous veins by dilating or enlarging the Schlemm’s canal using a microcatheter that illuminates and injects a sterile viscous gel into the canal.
It is considered a “Minimally Invasive Glaucoma Surgery (MIGS)” as it involves a small incision only, is a short, relatively safe procedure that does not involve the conjunctiva of the eye. No implants are placed in the eye.
If you are intolerant of glaucoma medications, have difficulty taking drops as prescribed, have a history of failed selective laser trabeculoplasty (SLT) treatments, or if it is difficult for you to commit to regular follow-up treatments, you may benefit from a MIGS procedure such as iTrack ab-interno canaloplasty. This procedure can be performed at the time of cataract surgery.
What are the risks?
General risks (common to other ocular surgical procedures) involved with the iTrack Ab-interno canaloplasty include:
- Insufficient reduction of eye pressure
- No change in number of glaucoma medications prescribed
- A spike in intraocular pressure
- Bleeding or infection in the eye
Specific risks involved with the iTrack Ab-interno canaloplasty include
- Stripping away of Descemet’s membrane, the internal layer of the cornea which can lead to visual impairment.
Are there any alternatives?
If iTrack™ ab-interno canaloplasty is unsuccessful, your ophthalmologist can still use medications, laser or perform other glaucoma surgery such as another MIGS or conventional trabeculectomy or tube surgery.
If combined with cataract surgery, the procedure should take 30-40 minutes and is a day surgical procedure. During the surgery your eye will be anesthetised. Post-surgery your ophthalmologist will prescribe eye drops to reduce inflammation and to prevent pain. Patients can resume normal, day-to-day activities soon following treatment.
Remember that managing glaucoma is a lifelong process: even after iTrack and other glaucoma treatments, you will need to continue to visit your ophthalmologist every three to six months.
PRESERFLO® MicroShunt
What is it?
PRESERFLO® MicroShunt is a tiny, soft, flexible stent that helps your eye drain excess fluid, may lower eye pressure, and prevent further vision loss. PRESERFLO® MicroShunt will not restore vision already lost to glaucoma.
How does it work?
PRESERFLO® MicroShunt is designed to drain excess fluid from your eye, which may lower eye pressure and prevent further vision loss.
Who is it suitable for?
PRESERFLO® Microshunt is suitable for patients with open angle glaucoma in whom medical and laser therapy have failed or are not suitable. It is not suitable for patients with narrow or closed anterior chamber angles.
What are the benefits?
Compared with traditional glaucoma surgeries, PRESERFLO® MicroShunt may result in fewer complications after surgery.
In the pivotal study, the majority of PRESERFLO® MicroShunt patients were medication-free at 12 months.1 Your physician will determine whether medications are required following implantation of PRESERFLO® Microshunt.
Before the Procedure
Your doctor will provide you with specific instructions prior to the operation. You will usually be asked to continue with all your usual medications including your glaucoma eye drops even on the day of surgery. You will likely have a period of fasting immediately before the surgery but again your doctor will provide you with the specific details. Be sure to follow instructions accurately and discuss associated risks, safety information, and questions you may have prior to surgery. For your safety, arrange to have someone take you home after surgery.
During the procedure
PRESERFLO® MicroShunt is a surgical device implanted into the eye for the management of glaucoma to help drain excess fluid out of the eye. The surgery is usually performed as a day procedure in an operating room under local anaesthesia. The procedure is less invasive than traditional glaucoma surgeries and may take less time to complete. Its size, shape, and fin help keep the PRESERFLO® MicroShunt stable and securely in place, and it is designed to resist degradation over time.
After the procedure
In the first week after surgery, you may experience symptoms including:
- Blurry vision
- Eye redness
- Eye swelling
These symptoms should go away. To help the recovery process, your surgeon may prescribe eye drops. Do not rub your eye or perform any strenuous activity, including heavy lifting or physical exercise, shortly after surgery.
What are the risks?
The potential risks of PRESERFLO® Microshunt are similar to those of a trabeculectomy, including infection risk that is lifelong, risk of haemorrhage inside the eye during the surgery and in the early postoperative period, intraocular pressure that is too low after the surgery due to over draining of intraocular fluid, droopy eyelid, and loss of vision. There is also a risk of poor positioning of the device and a need for repositioning. Fortunately, all these risks are low. Your surgeon will discuss the risks in detail with you prior to embarking on surgery. It is important that you understand the risks and ask questions to clarify if you do not.
Are there any alternatives?
The alternative treatment options are glaucoma eye drops, laser therapy, one of the other MIGS devices, or conventional glaucoma surgery. Your doctor will be able to explain each of these and whether they are suitable for you.
References:
1. Baker D, Barneby H, Moster M, et al. Ab-Externo MicroShunt versus Trabeculectomy in Primary Open-Angle Glaucoma. Ophthalmology. May 2021, doi: https://doi.org/10.1016/j.ophtha.2021.05.023 2. Pinchuk L, Riss I, Batlle JF, Kato Y, Martin JB, et al. The use of poly(styrene-block-isobutylene-block-styrene) as a microshunt to treat glaucoma. Regenerative Biomaterials. 2016;3(2):137-142
What is it?
The Paul Glaucoma Implant (PGI) is a non-valved medical-grade silicone aqueous shunt that consists of a large endplate (44.9mm in length and 23mm wide) and a soft 0.1mm tube.
How does it work?
PGI is an aqueous shunt that is placed into the eye to drain excess fluid from inside the eye to the outside via an end plate placed under the skin of the eye (conjunctiva).
Who is it suitable for?
PGI is suitable for patients who have had previous unsuccessful glaucoma surgery, glaucoma that is difficult to be controlled via medications and secondary glaucoma (including uveitic, neovascular and traumatic glaucoma).
What are the benefits?
The main benefit is to reduce eye pressure while at the same time minimising risk of complications after surgery. These risks include hypotony (eye pressure too low), corneal damage and tube erosion.
Before the procedure
Your doctor will provide you with specific instructions prior to the operation.
During the procedure
Your eye will be anaesthetised. An incision will be made and the PGI plate will be inserted and secured with stitches. An suture stent will also be inserted into the tube itself to prevent overdrainage of fluid; this helps to prevent hypotony after surgery. The tip of the tube will be placed inside the eyeball away from the cornea. The procedure usually takes between 60 to 90 minutes.
After the procedure
Your eye will feel blurred, uncomfortable and irritated for a few weeks after surgery. You will need to use anti-inflammatory and/or antibiotic eye drops after surgery, and your doctor will advise when to reduce or stop the drops.
Surgery may be needed again in some patients. Frequent check-ups will be required to monitor the pressure within the eye.
What are the risks?
Potential risks of PGI include infection, tube occlusion and exposure, eye pressure that is too low or too high, double vision, damage to the cornea, and prolonged blurred vision.
Are there any alternatives?
The Baerveldt, Molteno and Ahmed Implants are other aqueous shunt implants that can be used to reduce eye pressure.
MINIject ®
What is it?
MINIject ® is a soft, porous silicone device used to help drain fluid from the eye. It is 5mm in length and differs from other minimally invasive glaucoma surgery (MIGS) devices as it is not metallic. Only one device is implanted.
How does it work?
MINIject ® is placed in the eye as a minimally-invasive procedure. It drains fluid out of the eye into a natural outflow pathway between the choroid (blood vessel layer) and sclera (outer white layer of the eye). This is a different pathway to other MIGS devices. The porous material of the device allows the fluid to drain through the implant, reducing eye pressure.
Who is it suitable for?
MINIject® is for adults with open-angle glaucoma. It has a favourable short- and long-term safety profile. Due to the high efficacy of MINIject® in lowering the eye pressure, it is often recommended for patients who require further lowering of their eye pressure and, where their treating ophthalmologist determines, it may also be appropriate to reduce or stop the use of their eye drops.
What are the benefits?
MINIject ® significantly reduces eye pressure and sustains it over time. It may also reduce the need for use of glaucoma medication and further interventions. The MINIject® minimally-invasive procedure is safe and has a more rapid recovery than conventional glaucoma procedures. The implant cannot be felt or seen in the eye, and because the implant is made of silicone, it is MRI and X-ray safe.
Before the procedure?
Your ophthalmologist will provide you with guidelines and instructions, such as adding or discontinuing certain eye drops from your daily regimen.
During the procedure?
Your eye will be numbed during surgery and a small (2.2mm) incision will be made in the cornea. MINIject® will be inserted with a 0.5mm protrusion into the anterior chamber (front chamber of the eye) so that there is sufficient distance away from the cornea. The procedure usually takes between 15 to 30 minutes.
After the procedure?
Your ophthalmologist may provide some guidelines such as precautions when it comes to driving and returning to work. You will need to use eye drops after surgery to prevent inflammation and/or infection, similar to what is done after cataract surgery. Your ophthalmologist will advise when to reduce or stop these drops. Recovery time is approximately the same as after cataract surgery.
What are the risks?
MINIject® is generally safe, however risks include infection, temporary bleeding, damage to the cornea, eye pressure that is too low or too high, and device failure.
Are there any alternatives?
Alternative treatment options include eye drops, laser therapy, other MIGS devices, or conventional glaucoma surgery. Your ophthalmologist will discuss each of these options and decide which ones are suitable for you.



