Share
An Australian study exploring the mental and physical impact of visual field testing has identified workarounds that could make the experience more comfortable and less stressful. In doing so, patients, particularly those at risk or living with glaucoma, are likely to be more compliant with monitoring regimens, write Dr Jabelle Lu and Professor Graham Lee.
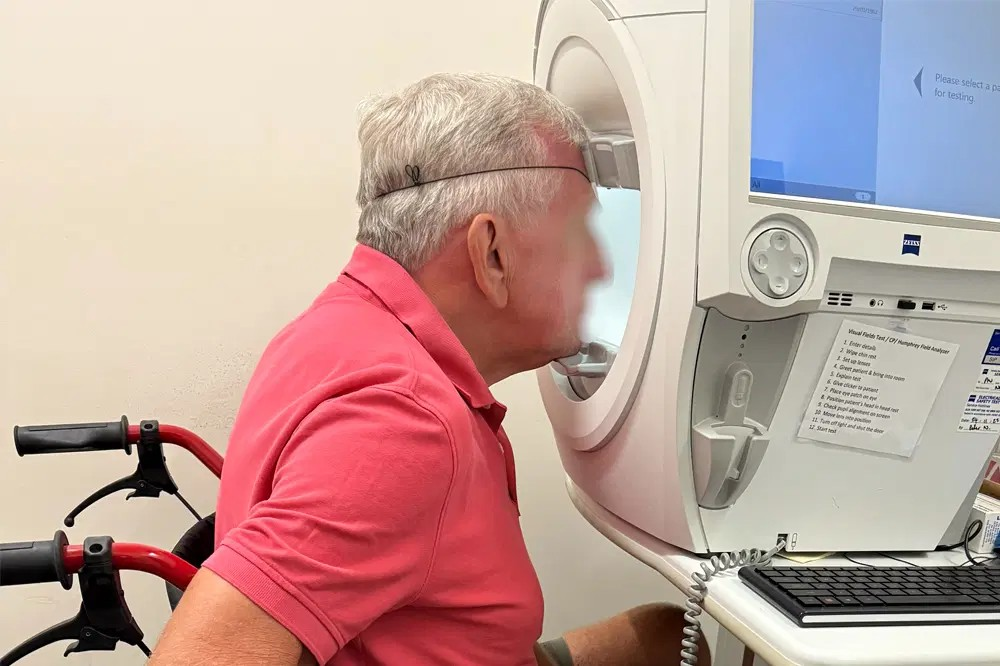
It is a familiar scene in ophthalmology clinics: patients seated at the visual field machine, fixating on a small central dot while responding to fleeting stimuli in their peripheral vision. For clinicians, this test is a cornerstone in glaucoma management, providing vital information about the state of a patient’s visual field, detecting disease progression, and guiding treatment decisions. For patients, however, it has gained a reputation as a stressful test of endurance.
A recent study investigating the visual field-testing experiences of 152 patients attending a private ophthalmology clinic in Brisbane has shed light on the mental and physical challenges associated with the testing process.1 The findings are particularly relevant for patients living with glaucoma, who make up a significant portion of those requiring this test, often repeatedly, throughout their lives.
… the combination of mental strain and pressure to perform well can make the experience of visual field testing deeply taxing
Decoding the Emotional Landscape
For those who have not experienced visual field testing first-hand, imagine staring at a central dot in a bright dome for minutes at a time, trying to detect small flashes of light appearing in variable intensities – some so faint that you question whether you merely imagined them. The test demands not only unwavering concentration, but also requires you to sit still and avoid shifting your gaze. Now, add the pressure of knowing that missing too many of these flashes could reveal the progression of your sight-threatening disease.
Indeed, the combination of mental strain and pressure to perform well can make the experience of visual field testing deeply taxing, as highlighted by this study. Specifically, anxiety and mental fatigue emerged as the most prevalent themes associated with negative visual field testing experiences. Over 27% of participants reported struggling to maintain focus throughout the test, often feeling mentally drained, frustrated, or, as one participant vividly described, “wrecked” by the end. Nearly one in five participants also described heightened stress, fearing they might miss stimuli and “fail” the test. For some, the rapid pace of the test was overwhelming. As one participant explained, “The dots come so quick, and you have to have that concentration and coordination”. Another shared, “I forget to breathe because I have to be so focussed, and I am scared to blink in case I miss a dot”.
Moreover, the uncertainty around whether they’ve accurately identified a stimulus adds another layer of stress. Some participants left the test feeling defeated, as though their ability – or inability – to spot stimuli reflected their competence or the progression of their disease. This misinterpretation can stem from a lack of understanding that a significant proportion of the test’s stimuli are designed to be missed, making it an inherently challenging test, even for those with normal vision.
Occasionally, the sense of defeat and frustration extended beyond the subjective experience of the individual, leading to disengagement with the test altogether. As one participant commented, “You just keep clicking the thing and hope for the best”.
Physical Discomfort and Ageing
Neck and back pain, along with increased fatigability, are common challenges faced by the ageing population. These physical issues can complicate the experience of visual field testing, which requires patients to maintain a fixed posture for a period of time. Several participants in the study reported having to endure pain in their neck and back throughout the testing process, with one participant noting that the discomfort had once become so intense that they were unable to complete the test.
Building a Better Testing Experience
While visual field testing devices continue to evolve, and alternative options become more accessible, improving the patient experience of visual field testing doesn’t necessarily require a complete technological overhaul. Small, patient-centred adjustments can make a significant difference in improving patient experience.
For instance, allowing patients to initiate breaks during the test, such as by holding down the clicker button, can help reduce mental fatigue and physical discomfort. This can also allow patients to have a sense of control over the process, potentially reducing feelings of frustration and apathy.

Pre-test education and clear communication are also critical. Many patients enter the test feeling unprepared and not fully understanding its difficulty. Explaining to patients that some flashes are designed to be missed, and reassuring them that the test is challenging for everyone – not just for those with glaucoma – can help alleviate performance anxiety and the perception of failure.
Clinics with the resources to invest in alternative devices could consider adopting head-mounted virtual reality (VR) visual field goggles. Unlike traditional visual field machines, these devices allow patients to undergo testing in more comfortable positions, such as sitting back in a chair or even lying down. VR goggles represent a promising solution for patients with physical limitations or chronic pain, as they can significantly improve comfort and accessibility.
Patients living with glaucoma already contend with the challenges of managing a sight-threatening condition, including the fear of vision loss and the rigours of ongoing treatment. While visual field testing remains an invaluable tool in glaucoma management, it is important to acknowledge that it can also be emotionally and physically taxing for the patient. By implementing patient-centred changes, clinicians can make a small yet meaningful step towards further supporting the patient along their glaucoma care journey.
Dr Jabelle Lu MD MMed (Ophthal) is a junior doctor with a strong passion for ophthalmology. With a deep interest in understanding the lived experiences of patients with chronic eye diseases, her work aims to integrate best clinical practice with patient-centred care.
Professor Graham Lee DMed (Res) MB BS (Qld) FRANZCO is a dual-fellowship trained subspecialist in glaucoma, corneal, and external diseases and has consulted in private and public clinics in Brisbane for over two decades. A co-founder of the International Ophthalmology Portal to promote high-quality in-depth teaching of ophthalmology, he has been published in peer-reviewed literature more than 130 times and has presented more than 250 lectures worldwide. He has received national and international awards.
Reference
Lu SJ, Girgis S, Shah P, Lee GA. Patient experience and barriers to the visual field test for glaucoma. J Glaucoma. 2024 Nov 1;33(11):835-840. doi: 10.1097/IJG.0000000000002477.
This article has been republished courtesy of Mivision



