Share
Greater knowledge of disease risk factors, new approaches to detection and monitoring, and innovative treatments are positively impacting glaucoma outcomes.

Over the past year we’ve seen a continued shift towards surgical/laser management of glaucoma, coupled with depot preparation medication trials rather than drop therapy. A major prospective trial looking at the efficacy of depot bimatoprost intracamerally has just finished recruiting (ARTEMIS 1) and two more are still underway (ARTEMIS 2 and ATHENA). Other similar trials are underway as well as assessment of an ocular ring releasing bimatoprost.1,2

Image 1: iStent Injection System
Should We Add Vitamin B3 To The Water?
The paper with the biggest potential therapeutic impact this year described the potentially protective role of Vitamin B3 in glaucoma. A team from the Jackson Labs in the US fed vitamin B3 to mice prone to ocular hypertension, resulting in a significant reduction in the risk of ganglion cell death. This effect was even greater than targeted gene therapy treating the proposed metabolic/inflammatory pathway implicated in the disease process.3 Small scale clinical trials have already started. Much like the findings from the Nurses Health Study and nitrates, there seems to be an increasing role for dietary and nutritional supplementation in preventing glaucoma and/or halting progression.4
Image 2: Cypass Micro-stent
Minimally Invasive Glaucoma Surgery
Undoubtedly in 2017, glaucoma clinical practice focused on minimally invasive glaucoma surgery (MIGS).
MIGS represents a broad group of small surgical devices characterised by minimal conjunctival dissection, short operating times, rapid recovery and a good safety profile. This is a rapidly expanding field with trans-trabecular devices (eg iStent, Glaukos), increasingly performed in conjunction with cataract surgery.
Other devices are available, with a growing body of supportive data, such as the Cypass (Alcon), which creates a cyclodialysis cleft and drains to the suprachoroidal space and the Hydrus microstent (Ivantis), a fenestrated curved tube that enters, passes through and dilates Schlemm’s canal.
Currently, Medicare restricts the use of these devices to only at the time of cataract surgery, although work is underway to expand the availability for the procedure to a wider body of glaucoma patients, and potentially allow stand-alone MIGS procedures.
There is still a scarcity of robust MIGS scientific data. A meta-analysis of all MIGS papers released up until 2016 found that while overall safety data from MIGS is reassuring, good head-to-head random clinical trials comparing MIGS devices to one another or to traditional glaucoma surgery is lacking.5 As clinicians in this field, it is imperative we collect quality local data that evaluates MIGS in real- world clinical practice, and audit through communal software platforms such as the Save Sight Registry.*
Hydrus was compared head-to-head with selective laser trabeculoplasty (SLT) in a small (n=56) case series. Hydrus resulted in a greater reduction in medication dependence than SLT at 12 months.6

Image 3: Hydrus Microstent
Filtration Surgery
Glaucoma filtration surgery (eg. trabeculectomy, tube surgery) involves creating an aqueous drainage pathway from inside the eye to the subconjunctival space. Some preliminary results have been released for the Primary Trab vs. Tube Study (PTVT) that attempts to settle the question as to whether a primary drainage tube may be better than trabeculectomy as a first surgical procedure for glaucoma. In a word, no.7,8 IOP control was better in the trabeculectomy group, especially in those with lower starting IOP. The complication rate was similar despite more early complications/interventions in the trabeculectomy group.
The Xen Gel Implant (Allergan) is a soft collagen implant that is inserted, ab interno, from the anterior chamber into the subconjunctival space creating a bleb. In many ways it is more similar to traditional filtration surgery than to other MIGS devices. It is increasingly used as an alternative to trabeculectomy, although quality head-to-head studies comparing Xen to trabeculectomy are few.
The Xen was shown to be effective in uveitic glaucoma, despite the potential for sight-threatening complications of hypotony, bleb infection9 or suprachoroidal haemorrhage10 (ie similar complications to a trabeculectomy).
Lasers In Glaucoma
The efficacy and safety of SLT in the treatment of open angle glaucoma (OAG) continues to be supported by the literature. SLT was evaluated in Afro-Carribeans with primary OAG (POAG) and found to have a 12 month success rate of 78 per cent.11 In Belgium, SLT was evaluated as replacement therapy for medically controlled OAG; it was able to completely replace medical therapy in 77 per cent of eyes after 18 months12 and improved treatment related quality-of-life (QoL)13 with similar efficacy between phakic and pseudophakic eyes.14However, when 24- hour IOP rhythm was evaluated by the contact lens sensor Triggerfish, SLT was not shown to alter the amplitude or pattern of the IOP rhythm.15
Angle Closure And Glaucoma
Angle closure is frequently missed, both among patients referred for cataract surgery who are often dilated without prior gonioscopy, and among patients with POAG who can develop phacomorphic angle closure with age. Two studies from Canada elegantly demonstrated this; of patients referred for cataract surgery, 1.5 per cent were found to have undetected narrow angles,16 and one in 11 patients, with a diagnosis of OAG referred to a tertiary glaucoma centre, were found to in fact have angle closure.17
Dysphotopsia is a rare but debilitating complication of laser peripheral iridotomy (LPI). Previous data suggested the frequency of this can be reduced by temporal placement of the LPI.18 However, a larger (n=595) Indian/US RCT found that location, LPI size, and amount of laser energy used did not affect the frequency of dysphotopsia reported.19
Another large Indian study confirmed that LPI hastens the development of cataract.20 These findings support the landmark EAGLE study that compared early clear lens extraction (CLE) to laser iridotomy in the management of primary angle closure glaucoma (PACG). CLE showed greater efficacy and was more cost-effective than laser iridotomy.21
Externally applied micropulse cyclophotocoagulation (M-CPC) is an alternative mode of laser delivery to continuous wave cyclophotocoagulation (CW-CPC). Micropulse has a high post- treatment inflammation rate (46 per cent after three months) and a similar but potentially lower complication profile than CW-CPC.22More head-to-head studies are required comparing micropulse to continuous wavelength and to endoscopic CPC to better elucidate this rapidly developing technology.
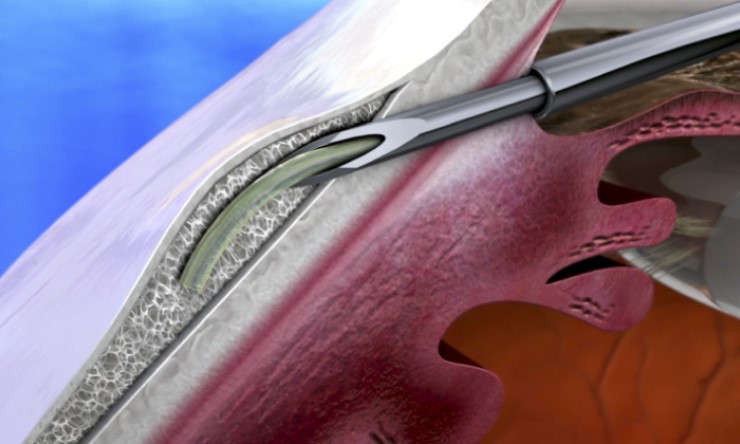
Image 4: Xen Gel Implant
Monitoring And Detection
We have yet to improve the 50 per cent undiagnosed glaucoma rate in Australia. However, new advances in diagnostic technology, a greater drive for optometry- led detection, and an emphasis on first- degree relative screening such as through the TARRGET study may improve the detection rate.
Australian-developed tablet-based perimetry has the potential to revolutionise glaucomatous monitoring, allowing home or waiting-room self-screening for glaucoma. It is easy to use and sensitive to glaucomatous progression.23,24
Three separate studies have confirmed the importance of central (eg 10-2) visual fields in glaucoma diagnosis to complement 24-2 fields; the latter might miss early glaucomatous defects. This trend persisted irrespective of the type of field machine used.25-27 Furthermore 10-2 changes had a greater impact on vision-related quality of life (QoL) than 24-2 changes.28
The frequency of monitoring for glaucoma patients continues to vex strained clinics. One study found twice yearly visual field testing had similar sensitivity to thrice yearly for detecting glaucoma progression, provided two quality baseline tests were available for reference.29 These findings support the UK Glaucoma Treatment Study, in which a few early visual fields established a firm baseline; this allowed sensitive detection despite greater intervals between later field tests.30
OCT-angiography (OCT-A) continues to be explored in glaucoma. Adding to vascular loss previously described at the optic nerve head, new studies have found macular vascular density declines in glaucoma.31,32 However this finding was not consistent; one study found the macular vessels were spared in glaucoma.33 In addition, the diagnostic sensitivity of OCT-A is lower than traditional OCT metrics (RNFL and MGC complex thickness).33
One drawback of OCT analysis glaucoma is a floor effect of the peripapillary RNFL (sensitivity is lost in advanced disease). In agreement with prior studies, the ganglion cell inner plexiform layer metric was again shown to be more sensitive for advanced glaucoma than the peripapillary RNFL and continued to demonstrate progression once the RNFL had reached its floor effect.34,35 More data has supported the water drinking test, finding IOP spikes induced by the water-imbibed challenge were predictive of future glaucomatous progression.36
The Genetics Of Glaucoma
The last few years have seen an explosion of genes identified in glaucoma pathogenesis. Novel loci include: for POAG (ABCA1, AFAP1, GMDS, PMM2, TGFBR3, FNDC3B, ARHGEF12, GAS7, FOXC1, ATXN2, TXNRD2); PACG (EPDR1, CHAT, GLIS3, FERMT2, DPM2-FAM102); and pseudoexfoliation syndrome glaucoma (CACNA1A).37 There are so many genes implicated that work is beginning to move towards better phenotyping of glaucoma for targeted gene studies, and studies looking at the functionality of these genes and interactions with each other (ie. is it combinations of gene anomalies rather than a single gene that is causative?). Stay tuned.
Health, Socioeconomic And Lifestyle Factors
Smoking was the smoking gun for glaucoma in 2017. A Spanish cohort population study of 16,797 participants over 8.5 years demonstrated a direct association between current smokers and glaucoma incidence, and the risk increased with number of pack-years.38
Additionally, a retrospective study looking at risk factors for rapid glaucoma progression showed rapid progressors were older, had significantly lower baseline IOP and central corneal thickness, and significantly higher rates of cardiovascular disease and hypotension.39 Further prospective study needs to be done to better understand the pathophysiology behind this finding.
A Taiwanese study evaluated the influence of different socioeconomic factors on vision-related quality of life in glaucoma. A lower education – but not income – affected QoL detrimentally, suggesting the importance of additional counselling for patients with a lower educational level to help them cope with the disease.40
“there seems to be an increasing role for dietary and nutritional supplementation in preventing glaucoma and/or halting progression”
Other Medical Therapies
Drug development for new glaucoma therapies has been slow but continues.
Rhopressa (Netarsudil 0.02 per cent) is a once daily topical agent with two mechanisms of action and two targets. Rhopressa targets rho-kinase (ROCK) and a norepinephrine transporter (NET). Trial results (ROCKET1-4) yet to be published seem promising. The most common side effect was mild redness of the eyes.
A combination product, Roclatan, is a once daily, combination of netarsudil 0.02 per cent + latanoprost 0.005 per cent made by the same company (Aerie Pharmaceuticals). Initial results from two trials (Mercury 1 and 2) also seem promising.
A new pathway for treatment was discovered this year that may also show promise. The angiopoietin-Tie2 system is crucial in the development and maintenance of Schlemm’s canal and hence IOP control. Antibody mediated activation of Tie2 resulted in an increase in drainage apparatus in Schlemm’s canal when injected in mice. Further development of this pathway may lead to a new IOP lowering agent in the future.37
Conclusion
As clinical and laboratory science marches forward, we must stay nimble in our approach to clinical practice, and translate the new knowledge into better, more efficient and more inclusive glaucoma care delivery to all patients.





