Share
New technologies and collaborative care are improving the quality of life of patients with glaucoma.
Glaucoma is one of the leading causes of irreversible blindness in the world, estimated to affect 66 million people worldwide and some 300 000 Australians.1,2 The majority of glaucoma patients present with progressive asymptomatic visual loss, with over 50% remaining undiagnosed.3 Annual costs of glaucoma to the health system in Australia are estimated to increase from $355 million in 2005 to $784 million by 2025.2 Management of this disease requires early detection, encouraging treatment adherence, improving patients’ quality of life and advancing medical research. To achieve this, strong collaboration is required between ophthalmologists, optometrists, orthoptists, pharmacists, general practitioners, patient advocacy groups like Glaucoma Australia and the Royal Australian and New Zealand College of Ophthalmologists, and funding bodies.
Advances In Early Detection
Glaucoma is characterised by progressive optic nerve thinning and corresponding loss of visual field. To prevent progression to vision impairment, early diagnosis is critical. One strategy to achieve early diagnosis is through identification of risk factors that predispose individuals to the condition. One of the most important and modifiable risk factors for glaucoma is elevated intraocular pressure; however, there is a high degree of intraocular pressure overlap in eyes with and without glaucoma. A second significant risk factor is ageing, which is common to many other neurodegenerative diseases.1 It is postulated that the optic nerve becomes more vulnerable to intraocular pressure injury with age; causes include vascular, mechanical and metabolic factors. A third significant risk factor is a family history of glaucoma, with first degree relatives having up to 10-fold increase in risk of developing glaucoma, and large scale genetic analysis has identified important genetic loci that confer glaucoma risk.4 For early detection, National Health and Medical Research Council guidelines recommend that people over the age of 50 years should have a comprehensive eye examination regularly, or over 40 years for people with a family history of glaucoma or other risk factors such as African descent.5
Technological advances have also provided clinicians with improved ways of earlier detection of glaucoma or disease progression. Early detection of disease progression in glaucoma is important because optic nerve damage is currently irreversible and, when progression occurs, clinicians must consider escalation of treatment. One of the most important advances is the optical coherence tomography (OCT), which uses laser interferometry to allow detailed non-invasive visualisation of the retina and optic nerve. OCT can detect thinning of the optic nerve caused by glaucoma, even in early disease progression. Higher resolution OCT of optic nerve microvasculature, known as OCT angiography, is yet to be used in mainstream practice; however, it has great potential for understanding the underlying mechanism of disease in glaucoma.
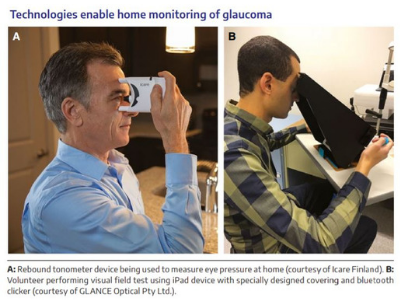
A new concept in early detection of glaucoma progression is home monitoring. An early study has shown eye pressure monitoring at home can be performed using a handheld tonometer by patients at risk of disease progression.6 Software for visual field monitoring on tablet devices allows patients to reliably and regularly test their own visual fields at home7 (Box). Lower cost portable OCT devices for use in the home are also currently under development. Data collected in the home (including eye pressure, visual field, fundus photographs and OCT images) may in the future be assessed by artificial intelligence to identify patients with glaucoma progression, providing precision medicine to those in most need of treatment. Artificial intelligence can already identify the risk of glaucoma from retinal fundus photographs with a high degree of accuracy.8 Future large scale studies are required to demonstrate whether home monitoring will lead to earlier detection of disease progression compared with standard clinic reviews.
Recent Improvements In Treatment
All current glaucoma treatments, such as topical eye drops, laser treatment or surgery including minimally invasive glaucoma surgery (MIGS), either reduce aqueous production, improve outflow, or both. Many studies indicate that adherence to topical glaucoma drops is generally poor, varying from 24% to 59%.5 Patients with glaucoma often require treatment for several decades for a disease that is largely asymptomatic; it is therefore important that treatments have minimal side effects and are cost-effective to both patients and the community. This can be improved by using combination eye drops, drops containing less harsh preservatives, or reducing preservative exposure by using preservative-free single dose drops. Topical glaucoma medications can also cause other local and systemic side effects. General practitioners can liaise with the patient’s ophthalmologist if side effects are identified as problematic.
In response to potential side effects from topical glaucoma medications, selective laser trabeculoplasty is increasingly used as an adjunct treatment or as first line treatment. This in-office procedure can result in eye pressure lowering similar to that of glaucoma eye drops, and repeat treatments can be performed. Many newly diagnosed open-angle glaucoma patients now elect to have selective laser trabeculoplasty instead of starting eye drops;9 however, the long term comparative cost and quality of life consequences are currently being investigated.10
Glaucoma management worldwide is currently undergoing a process of dramatic change with the introduction of MIGS to the repertoire of glaucoma treatment. MIGS uses an implanted device to bypass outflow restrictions in the eye, allowing the procedure to be performed quicker, causing less tissue trauma and having better safety than traditional drainage surgery. Commonly used MIGS devices in Australia are the transtrabecular bypass stent and a specially designed gelatin stent that drains aqueous humour from the anterior chamber to the subconjunctival space (similar to a traditional glaucoma filtration operation) without an incision in the conjunctiva. Because of the minimally invasive nature of these procedures, glaucoma specialists have a lower threshold for using these devices for patients whose glaucoma is inadequately controlled, particularly for patients affected by eye drop side effects. The devices currently used in Australia show varying degrees of reported success in the medium term.11 Further investigation is required to examine the long term success of MIGS devices on quality of life for patients.
Patient-Oriented Management
While there are many exciting advances in glaucoma treatment, their effectiveness will be limited if there is inadequate patient engagement, or if they do not adequately address quality of life outcomes. Clinicians therefore need to discuss diagnosis and treatment with patients to allay their fears and encourage treatment adherence. Glaucoma Australia is an important patient support organisation whose mission is to eliminate glaucoma blindness by promoting early detection and improved treatment adherence, and supporting ongoing management. Glaucoma Australia has a comprehensive referral response pathway with proven effectiveness in educating and supporting patients through all stages of their journey.12 This includes individual phone support from diagnosis and after reviews, tailored e-communications throughout the year, helping in areas of eye drop application and technique, adherence, research, and family and collaborative care.
Future Research
New research in glaucoma focuses on ways to protect the optic nerve from further damage independent of eye pressure (neuroprotection) and on ways of regenerating the damaged optic nerve (neuroregeneration). One area of neuroprotection aims to improve energy supply to the nerve. In animal studies, diet restriction, which among other effects improves mitochondrial function, has been shown to protect ageing optic nerves from pressurerelated damage,13 as has vitamin B3 (nicotinamide) supplementation in an animal model of glaucoma.14 However, whether these findings will lead to effective long term treatments in humans remains to be seen.
Neuroregeneration that results in the restoration of patients’ vision is one of the ultimate challenges for glaucoma research. Some molecular targets could simultaneously enhance both retinal ganglion cell survival and axon growth. The most promising of these are mediated by neurotrophins; however, the challenges of regenerating cell body, guiding regenerating axons along the correct pathway, and long term sustained delivery of neurotrophins inside the eye are substantial.15 Developments in stem cell technology may help overcome some of these challenges, although these are still some time away from clinical application.
While these and many more exciting new developments in eye research are on the horizon, funding for research is limited. The annual success rate for funding from the National Health and Medical Research Council for high quality project grants is about 10%, and many projects depend on smaller funding sources such as the Ophthalmic Research Institute of Australia, the research arm of the Royal Australian and New Zealand College of Ophthalmologists. It is hoped that the government initiative of the Medical Research Future Fund will improve funding for ophthalmic research projects in the future.
Conclusion
The management of glaucoma is undergoing many new and exciting developments. Advances in the diagnosis, as well as medical and surgical treatments, are paving the way for patients to maintain their vision with glaucoma. A collaborative clinical care pathway, supported by Glaucoma Australia’s tailored patient-centred management plan, delivers a framework for best practice patient outcomes that improves disease knowledge, treatment adherence, ongoing support and future research. These advances are important in tackling the expected increase in the incidence and prevalence of glaucoma over the next decade. Greater funding for research, patient advocacy and public awareness programs are required to ensure that the future needs of glaucoma management are met.
Authors:
Yu Xiang George Kong - Royal Victorian Eye and Ear Hospital, Melbourne, VIC. Centre for Eye Research Australia, Melbourne, VIC.
Annie Gibbins - Glaucoma Australia, Sydney, NSW.
Anne Brooks - Royal Victorian Eye and Ear Hospital, Melbourne, VIC. Centre for Eye Research Australia, Melbourne, VIC.
Acknowledgements: Yu Xiang George Kong is supported by an Ophthalmic Research Institute of Australia New Investigator Grant. Competing interests: Yu Xiang George Kong is Director of GLANCE Optical Pty Ltd. Provenance: Commissioned; externally peer reviewed.
References:
1 Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90: 262–267.
2 Dirani M, Crowston JG, Taylor PS, et al. Economic impact of primary open-angle glaucoma in Australia. Clin Exp Ophthalmol 2011; 39(7): 623–632. Epub 2011/06/03.
3 Keel S, Xie J, Foreman J, et al. Prevalence of glaucoma in the Australian National Eye Health Survey. Br J Ophthalmol 2018; https://doi.org/10.1136/bjophthalmol-2017-311786 [Epub ahead of print].
4 Shiga Y, Akiyama M, Nishiguchi KM, et al. Genome-wide association study identifies seven novel susceptibility loci for primary open-angle glaucoma. Hum Mol Gen 2018; 27: 1486–1496.
5 National Health and Medical Research Council. NHMRC guidelines for the screening, prognosis, diagnosis, management and prevention of glaucoma. Canberra: NHMRC, 2010.
6 Sood V, Ramanathan US. Self-monitoring of intraocular pressure outside of normal office hours using rebound tonometry: initial clinical experience in patients with normal tension glaucoma. J Glaucoma 2016; 25: 807–811.
7 Anderson AJ, Bedggood PA, George Kong YX, et al. Can home monitoring allow earlier detection of rapid visual field progression in glaucoma? Ophthalmology 2017; 124: 1735–1742.
8 Li Z, He Y, Keel S, et al. Efficacy of a deep learning system for detecting glaucomatous optic neuropathy based on colour fundus photographs. Ophthalmology 2018; 125: 1199–1206.
9 Katz LJ, Steinmann WC, Kabir A, et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomised trial. J Glaucoma 2012; 21: 460–468.
10 Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Laser in Glaucoma and Ocular Hypertension (LiGHT) trial. A multicentre, randomised controlled trial: design and methodology. Br J Ophthalmol 2018; 102: 593–598.
11 Lavia C, Dallorto L, Maule M, et al. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PloS One 2017; 12: e0183142.
12 Skalicky SE, D’Mellow G, House P, et al. Glaucoma Australia educational impact study: a randomised short-term clinical trial evaluating the association between glaucoma education and patient knowledge, anxiety and treatment satisfaction. Clin Exp Ophthalmol 2018; 46: 222–231.
13 Kong YX, van Bergen N, Bui BV, et al. Impact of aging and diet restriction on retinal function during and after acute intraocular pressure injury. Neurobiol Aging 2012; 33(1126): e1115–1125.
14 Williams PA, Harder JM, Foxworth NE, et al. Vitamin B3 modulates mitochondrial vulnerability and prevents glaucoma in aged mice. Science 2017; 355: 756–760. 15 Calkins DJ, Pekny M, Cooper ML, et al. The challenge of regenerative therapies for the optic nerve in glaucoma. Exp Eye Res 2017; 157: 28–33.



