Share
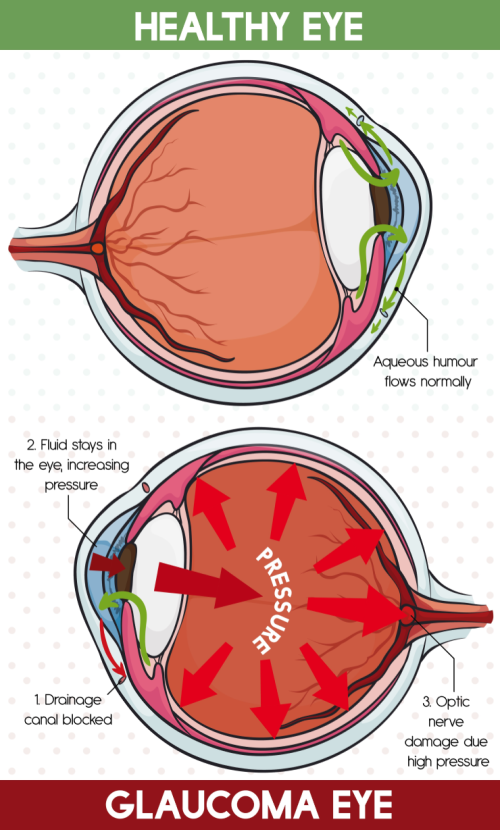
Glaucoma is a neurodegenerative eye disease. It is also called the "silent killer of eye sight" because it causes no pain or symptoms until significant portions of peripheral vision is lost. In other words, by the time symptoms appear, a significant amount of ganglion cells have already died. Since the nerve fibres of ganglion cells form the optic nerve, after the death of ganglion cells, optic neuropathy and then defects of the visual field follow.
Recently, there has been some exciting advancements which could potentially yield earlier detection of glaucoma. For example, a new real-time imaging technique called Detection of Apoptosing Retinal Cells was used to label dying human retinal cells in vivo (i.e. in the living body) with a fluorescent dye (Cordeiro et al., 2017). Also a group from Korea (Kim et al., 2017) developed a new contact lens which continuously measures glucose and intra-ocular pressure. The contact lens was safely tested on a rabbit and on cow eyes. Clinical trials on humans would be the next step. Both aforementioned techniques are non-invasive.
So is it possible to detect glaucoma even earlier? The answer is yes - by identifying molecular markers that predict or measure neurodegeneration in glaucoma. A recent American study by Ban and colleagues (2017) found the expression of one gene Gdf15 in mice, tested from a pool of 88, was increased after acute injury to the optic nerve. A significant increase in growth differentiation factor 15 (GDF15) protein levels in aqueous humour was also observed in these animals. The study confirmed that ganglion cells are the main source of GDF15 that diffuses to the aqueous humour. Similarly, Gdf15 gene expression and GDF15 levels were significantly elevated in a murine chronic glaucoma model (using DBA/2J mice) and in rats. One might ask: ‘Does it mean, GDF15 levels are too elevated in aqueous humour of glaucoma patients?’ The group took on the opportunity of patients with primary open angle glaucoma (POAG) who had undergone surgical treatments and collected one small sample (50-100µL) of aqueous humour from each patient. Indeed, GDF15 levels were increased. Further, the study stated that ‘elevated GDF15 levels are significantly associated with worse functional outcomes in glaucoma patients, as measured by visual field testing’.
It is important to note some of the limitations of the above study. For instance, glaucoma is generally a chronic disease, but the study was based on the acute injury of optic nerve by pinching. The other limitation is the use of DBA/2J mice as a chronic model, which is a model for pigmentary glaucoma rather than a model for primary open angle glaucoma. Nevertheless, the reported findings have made some progress in the early detection of a "silent killer of eye sight".



