Share
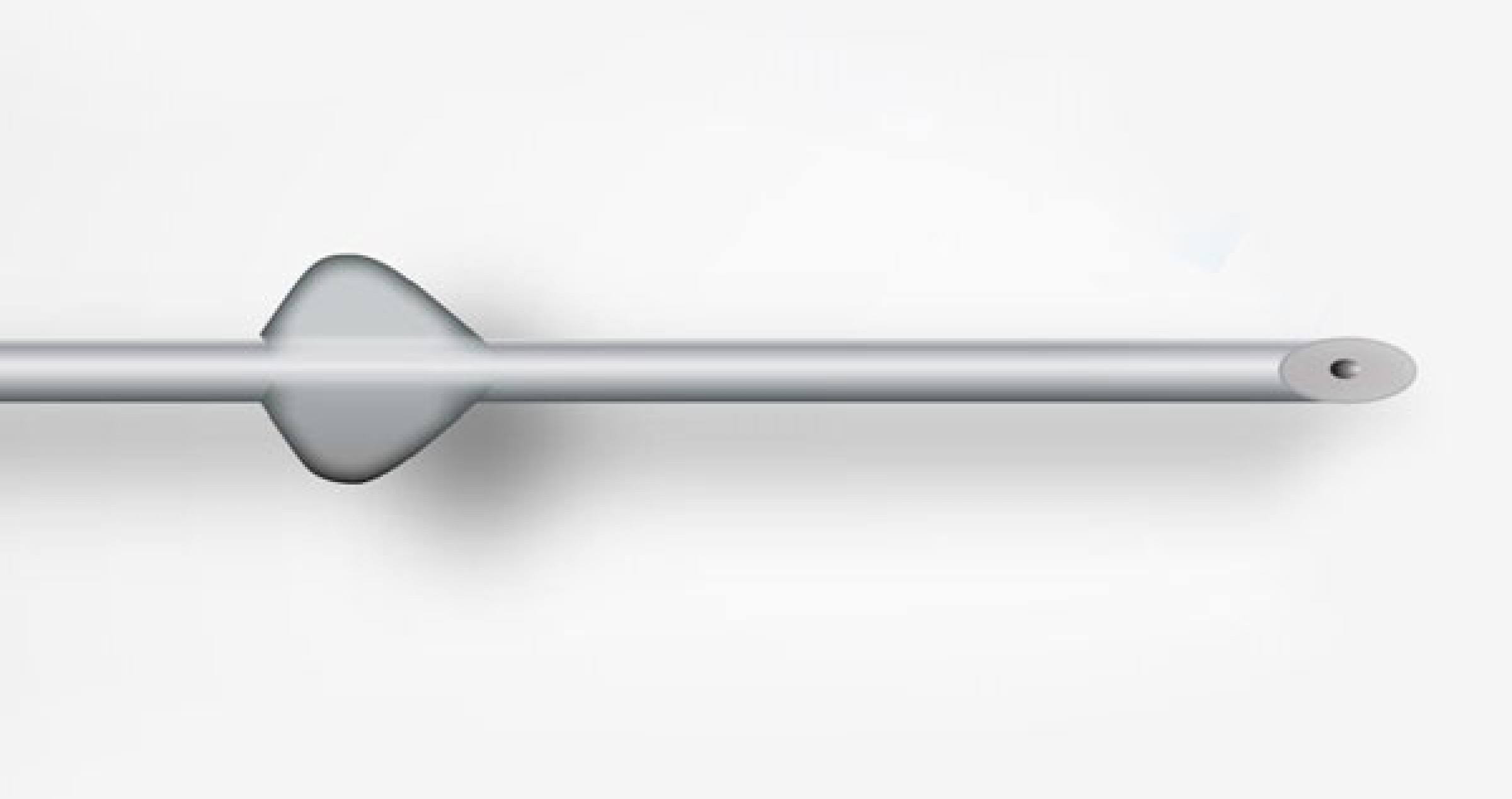
PreserFlo microshunt (Santen), a new minimally invasive glaucoma surgery (MIGS) device that performs in a similar way to a trabeculectomy, has been implanted in Australia for the first time.
Unlike many MIGS devices, the PreserFlo microshunt has capacity to produce a large pressure decrease, and therefore may be suitable for a wide range of glaucoma patients, including those with advanced glaucoma.
Formerly known as the InnFocus MicroShunt, five PreserFlo devices were implanted by Associate Professor Mitchell Lawlor (Sydney Eye Surgeons) using the Australian Therapeutics Goods Administration (TGA) special access scheme. Santen is currently applying for US Food and Drugs Administration (FDA) approval, and subject to patient data, Professor Mitchell hopes that FDA approval will be followed soon after with an application for Australian TGA approval.
Unlike other MIGS procedures (except the Xen implant), the PreserFlo would be available for implant independent of cataract surgery, as it involves a full thickness bypass through the trabecular meshwork into the subconjunctival space.
Positive Trial Results
A clinical trial, yet to be published, compared the PreserFlo procedure head to head with trabeculectomy and showed positive results.
“The great thing was this study compared a MIGS device with trabeculectomy – most compare MIGS against cataract, so this really was comparing against the gold standard,” said A/Prof Lawlor.
“The results demonstrated that although the PreserFlo did not lower intraocular pressures (IOPs) as much as a trabeculectomy, on average there was still over a 30% reduction in pressure, an important clinical metric we use for progressive or advanced glaucoma patients. Importantly, the rate of hypotony was much less with PreserFlo, making it potentially a safer procedure long term.”
The prospective, randomised controlled, singlemasked study found that patients implanted with PreserFlo had a mean diurnal IOP reduction from 21.1 ± 4.9 mm Hg to 14.2 ± 4.4 mm Hg at month 12 compared with 21.1 ± 5 mm Hg to 11.2 ± 4.2 mm Hg in the trabeculectomy group.1 Patients in both groups were able to reduce their medications from an average of three medications at screening to 0.6 in the Preserflo group and 0.3 in the trabeculectomy group. By month 12, 71.6% of Preserflo patients were medication-free compared with 84.8% in the trabeculetomy arm. The rate of hypotony was 51.1% in the trabeculectomy arm compared with 30.6% in the PreserFlo arm1.
May Help More Advanced Disease
A/Prof Lawlor said surgeons have been looking for some time for a MIGS device less invasive than trabeculectomy, that could still reliably treat patients with more advanced disease.
“Trabeculectomies are not without risk, especially for surgeons who don’t do many of them. They are a less predictable procedure than many current MIGS devices, and there is a greater risk of hypotony. If real-world data on PreserFlo matches the early trial data, this device may be a good alternative to trabeculectomy, at least in some patients. This is especially the case for patients at high risk of hypotony from trabeculectomy,” he said.
Faster Recovery
Having implanted five PreserFlo devices in Australia at the time of going to print, A/ Prof Lawlor said he has been impressed by the procedure, which he described as emulating a trabeculectomy – you make a conjunctival dissection, treat with mitomycin, and then create a 1 mm wide pocket through which the microshunt passes into the anterior chamber.
He said the procedure itself is forgiving. “You get good visibility of where the PreserFlo is sitting in the subtenons space, and can confirm the shunt is not embedded in the tenons layer. Because you’re working with a 1 mm wide incision as compared to the larger incisions required for a trabeculectomy, if you find the PreserFlo is not perfectly positioned, you can easily create a new pocket to adjust this.
“Another benefit of the small incision is that vision recovery appears faster. All five patients who have had surgery in Australia to date have not had any decrease in their visual acuity compared with preoperative values.”
Professor Mitchell said the initial patients he implanted have been added to the Fight Glaucoma Blindness! Registry (FGB!) – a collaborative project of Australian and New Zealand glaucoma specialists, with an interest in measuring real-world outcomes of MIGS devices. The registry will help to determine whether new treatments work, in which patients each device is most beneficial, and ultimately whether each device is cost-effective. Their progress will be closely followed.
“We implanted four patients without cataract and one patient in conjunction with cataract surgery. The goal is to ensure the procedure is safe, make sure vision is not affected, and reduce pressures by an appropriate amount for each patient. Whether there is any difference between combining with cataract or standalone procedures will be very interesting, and tracking via the FGB! registry will allow us to monitor this.”
Reference:
1. www.healio.com/ophthalmology/glaucoma/news/ online/%7B14858e53-65ba-4d44-a02a-67c757b2d6e2%7D/ de-128-microshunt-reduced-iop-medications-in-study




