This article looks at those medications that we take for other health conditions and their role in elevating the eye pressure, which may eventually lead to glaucoma. Sometimes the eye pressure can decrease once these medications are ceased, without any development of glaucoma. Most medications are safe in glaucoma, but there are some to be mindful of. If you have any concerns about the medications you are taking or about to start, then speak to your ophthalmologist.
There are many different types of glaucoma. However, most glaucomas can be divided into two categories: open-angle glaucoma where the drain of the eye is wide open, and closed-angle glaucoma where the drain of the eye is partially or fully obstructed. Whether the drain of the eye is open or closed is important when we are examining medication-induced glaucoma. This is because a medication can make your open-angle glaucoma worse or your angle-closure glaucoma worse. However, certain medications can create closed-angle glaucoma regardless of the type of glaucoma you have. These reactions are called ‘idiosyncratic’ or random individual reactions.
Your eye doctor can let you know if your type of glaucoma fits into either of these groups. Brand names are not used in this document, so look for the ‘generic’ name for the medication. One medication may have several brand names. You will find that most medications have the generic name or active ingredient listed on the box or information leaflet.
Your eye health professional is the best point of contact if you have been prescribed these medications. They can work with you and your prescribing doctor to check if you are at risk, and if the medication can be continued or should be ceased.
Open-Angle Glaucoma
Steroids
Corticosteroids, or steroids, can raise eye pressure, especially in those persons who have open-angle glaucoma, first-degree relatives of those with open-angle glaucoma, elderly and young (<6 years) persons, those with type 1 diabetes and those with high myopia (short-sightedness). All types of steroid formulation such as oral, inhaled or topical (drops or cream) can raise the eye pressure. A study that looked at nasal spray formulation of steroids demonstrated that there was not an increased risk of elevated eye pressure with this method of taking steroids.
Most patients will not have symptoms from elevated eye pressure associated with steroid use. If glaucoma develops, it may be years or decades before the vision loss becomes detectable by the patient. Very occasionally if the pressure is high enough to damage the cornea (front window of the eye), the patient may get blurring of the vision, but this is rare.
Corticosteroids are a useful medication in the treatment of many conditions, even life-threatening ones. We recommend that patients who are taking this medication, and have risk factors for glaucoma (see above) obtain a check-up from an eye health professional before and during treatment with steroids. The eye professional can assess them during treatment with steroids to ensure any elevated eye pressure can be detected early and treated. If elevated pressure occurs, treatment with pressure-lowering medications, laser or surgery as well as reduction in dose or duration of steroid use, changing formulation or cessation of steroids are all possible therapeutic options.
Anti-Cancer Medication
Docetaxel and paclitaxcel are medications used to treat some cancers. They can elevate the eye pressure.
Oncologists (cancer doctors) always send patients to an eye health care professional for an eye check after they commence a wide variety of cancer medications. If you are worried or haven’t been for a check-up, speak to your general practitioner, oncologist or local optometrist.
Anaesthetic agents
Some medications used in general anaesthesia such as succinylcholine and ketamine can raise eye pressure, though it is usually temporary and does not cause permanent harm.
Closed-Angle Glaucoma
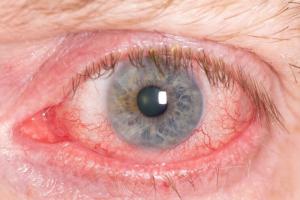
A large number of medications can precipitate closed-angle glaucoma. Closed-angle glaucoma causes the drain in the eye to block completely resulting in very high eye pressures, blurry vision, haloes, pain, red eye and nausea and vomiting. This can result in loss of vision and can be difficult to treat. Treatment usually involves laser, topical and oral medications, but may involve surgery as well.
People with narrow angles are most risk. This can be checked by your eye health professional. Those at risk of having narrow angles include: race (Asians, Inuit Eskimos and Hispanics), older age, female gender, hyperopia (far-sightedness or wearing plus glasses that magnify objects) and a family history of closed-angle glaucoma. Certain medications (sulpha-drugs) can produce rare idiosyncratic closed-angle glaucoma even in persons without narrow angles or a predisposition to narrow angles.
People with narrow angles may already be treated with a laser peripheral iridotomy. In this case they are at very low risk of developing sudden closed-angle glaucoma with the medications described below and can in most cases safely take these medications. If in doubt, it is best to check with an eye health care professional. However, people with undiagnosed narrow angles are most at risk of developing sudden closed-angle glaucoma. It is important for all adults to get an eye health check-up every 2 years.
Direct and Indirect Adrenergic Agents
Direct and indirect adrenergic medications include: phenylephrine, epinephrine, ephedrine, dipivefrin, naphazoline, salbutamol, albuterol, terbutaline, amphetamines, monoamine-oxidase inhibitors (tranylcypromine, phenelzine), apraclonidine drops and cocaine.
These medications or drugs can dilate the pupil and this can cause the iris (coloured part of the eye) to seal against the lens blocking orderly flow of fluid inside the eye. The fluid can’t get from the back to the front of the eye. This causes pressure behind the coloured part of the eye to rise narrowing the front of the eye and drain until it closes, which leads to the signs and symptoms such as pain and haloes, described above.
Anti-Cholinergic Agents
Anti-cholinergic drugs include: tropicamide, atropine, cyclopentolate, ipratropium bromide. Tricyclic and tetracyclic anti-depressants such as amitriptyline, imipramine, clomipramine are weak anti-cholinergics. Selective serotonin reuptake inhibitor anti-depressants such as venlafaxine, paroxetine, citalopram, escitalopram and fluvoxamine also have weak anti-cholinergic effects. Some anti-psychotics have even weaker anti-cholinergic effects and for closed angle glaucoma to result, usually need to be taken with another anti-cholinergic. These medications include trifluoperazine, perphenazine and fluphenazine.
These medications also cause closed angle glaucoma by the method described above. Drops such as tropicamide, atropine and cyclopentolate cause the iris to swell also which also can help to create an environment where closed-angle glaucoma is more likely to occur.
Botox injections
Botulinum Toxin Injections can cause pupil dilation when injected close to the eye. This can precipitate closed-angle glaucoma in the aforementioned way, in high-risk individuals (those with narrow angles).
Cholinergic agents
Pilocarpine is an eye pressure lowering drop that has been around for some time. It is still frequently prescribed by ophthalmologists. Pilocarpine constricts the pupil. But it also brings the lens and iris forward which can block the drain of the eye, causing closed-angle glaucoma.
Sulfa-Drugs
Such drugs include: trimethoprim-sulfamethoxazole, topiramate, acetazolamide, hydrochlorothiazide and cotrimoxazole.
These medications don’t dilate the pupil but they still cause closed-angle glaucoma. They swell the structures in the back of the eye. These swollen structures push the lens and iris forward, thereby blocking the drain of the eye (closing the angle).
Topiramate is a medication used for migraines and weight loss. There have been many case reports of closed-angle glaucoma from this medication.
These medications usually cause closed angle glaucoma in both eyes of children and adults. Typically, the glaucoma occurs within the first 3 weeks of use and treatment includes stopping the medication. Significant vision loss has been reported in some patients who develop sudden closed-angle glaucoma with these medications.
Anti-histamines
Promethazine has been shown to have weak anti-cholinergic activity and can cause closed-angle glaucoma by causing swelling of the structures in the back of the eye.
Gastrointestinal Medications
Cimetidine and ranitidine can also raise the eye pressure through their weak anticholinergic effects.
Anti-Parkinson medication
Such drugs include cabergoline, which can induce the structures at the back of the eye to swell up and thereby result in closed-angle glaucoma.
Trihexyphenidyl and orphenadrine have also be known to cause closed-angle glaucoma.
Cardiac agents
Disopyramide is used for heart rhythm abnormalities, and can cause closed-angle glaucoma.
Anticoagulants
Blood thinners may cause a big bleed in the back of the eye (vitreous haemorrhage, subretinal haemorrhage or suprachoroidal haemorrhage). The blood pushes the structures in the front of the eye forward, blocking the drain of the eye. However, this occurrence is quite rare and it is not recommended that you stop the anti-coagulant due to this rare risk. Overtreatment with anticoagulants, wet age-related macular degeneration and a small eye are risk factors for this rare condition.
Once the bleed occurs, treatment is difficult and requires stopping the anticoagulant to protect the fellow eye.
Anaesthetic Agents
Some of the aforementioned agents may be used during surgery which can precipitate closed-angle glaucoma. The glaucoma is often detected when the patient awakes after general anaesthesia.
References
1. Ahmadi N, Snidvongs K, Kalish L, Sacks R, Tumuluri K, Wilcsek G, Harvey R. Intranasal corticosteroids do not affect intraocular pressure or lens opacity: a systematic review of controlled trial. Rhinology 2015; 53:290-302
2. Razeghinejad MR, Myers JS, Katz LJ. Iatrogenic glaucoma secondary to medications. Am J Med 2011;124:20-25
3. Martin E, Patrianakos T, Giovingo M. Medication induced glaucoma. Disease-a-Month 2017;63:54-57
4. Khurana AK, Khurana B, Khurana AK. Drug-induced angle-closure glaucoma. J Curr Glaucoma Pract. 2012;6(1):6-8