Share
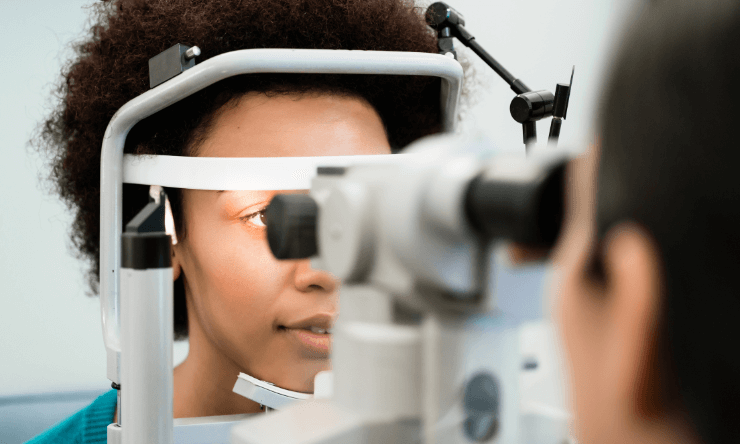
A new research project examining the proteins that circulate in the eye’s fluids has the potential to pave the way for a test to diagnose glaucoma that doesn’t rely on intraocular pressure.

Contrary to what many of us think, high pressure inside the eye does not define glaucoma and researchers want to know if the proteins circulating in the fluid of our eyes might.
While some patients do have classic high pressure inside the eye, the reality is others with glaucoma don't, says Dr. Ashok Sharma, proteomics and bioinformatics expert in the Center for Biotechnology and Genomic Medicine and Department of Population Health Sciences at the Medical College of Georgia at Augusta University.
Since glaucoma, a leading cause of blindness worldwide, often has no clears symptoms in the early stages, by the time a patient notices they have a problem they can have significant optic nerve damage and vision loss.
Now researchers are working to associate the proteins present in the eye’s fluid with the structural damage to the eye that is caused by glaucoma. Their goals are to find a better way to diagnose glaucoma, monitor its progress and maybe find new treatment targets. If they do, our tears may one day provide the fluid needed to perform such tests.
Sharma is the lead researcher who has been awarded a US$1.5 million (AU$2.1 million) grant from the National Institutes of Health to undertake this research project. Over the next four years researchers will examine and compare the fluid of the 200 patients with glaucoma with 400 patients with cataracts serving as control group.
Researchers are comparing the protein profile in the millionth of a liter of fluid, or aqueous humor, found in the eye - and removed as part of surgery - with clinical data, like images of a misshapen optic nerve, and other demographic and health data like age and race, to begin to write a proteomic signature for glaucoma.
"Probably half the people who have glaucoma do not have intraocular pressures above average," says Dr. Kathryn Bollinger, ophthalmologist, glaucoma specialist and retinal cell biologist in the MCG Department of Ophthalmology and the Culver Vision Discovery Institute, and a study co-researcher.
Conversely, some with what is considered high pressure don't have the potentially blinding condition. While the bottom line is damage to the neurons in the eye, the level of intraocular pressure that causes damage varies in different people, she says.
"That is part of the reason why these studies are so important, because we don't have a clear diagnostic indication for glaucoma based simply on intraocular pressure," Bollinger says.
"After we find a patient actually has glaucoma, we would like to classify them as adequately controlled and therefore stable rather than progressing," add Dr Lane Ulrich, ophthalmologist in the MCG Department of Ophthalmology and James and Jean Culver Vision Discovery Institute at AU, and a study co-researcher. "So we are looking for a good way to not only identify these patients but also to monitor them better."
While exactly where ocular proteins come from and what they do is largely a mystery, it is clear they are part of the microenvironment of glaucoma that should provide good clues about what is occurring at the molecular level, Sharma says.
"The aqueous humour has a lot of molecular information because it is in contact with tissues in the eye and there are proteins coming in and out, and all those molecules might be related to function," Sharma says.
Ophthalmologists routinely check eye pressure as a part of the eye exam and look in the back of the eye at the optic nerve for these classic shape changes that indicate it's under too much pressure. When they see changes, they get images to further confirm and study those changes.
"I usually tell patients it's sort of like a volcano, it's got a crater and then there is an edge of the volcano. In glaucoma, the crater gets bigger and bigger and bigger," Dr Ulrich says.
Like people themselves, some individuals' nerves can handle pressure better than others and you can't tell who they are by looking.
"We see patients all the time who have vision loss due to glaucoma that, if recognised earlier, could have been prevented," Bollinger says. "That is the idea here, to identify a signature that indicates early on that a particular person is either predisposed to developing glaucoma or they are not."
"This kind of study will allow us to really pinpoint people and to target our treatment toward people who need it," she says.
Glaucoma typically first affects peripheral vision; advanced disease causes total vision loss and is a leading cause of irreversible blindness worldwide. Treatments include eye drops that reduce pressure by reducing the production or increasing the outflow of aqueous humor. Surgery including laser can also improve outflow.
While glaucoma is a risk for everyone, especially as we age, it is a higher risk for blacks over age 40 and people with a family history. Associated risks include hypertension, diabetes, tobacco use and long-term use of corticosteroids.